Our microbiome plays an important role in our ability to overcome health issues. A healthy biome can make you resilient to these challenges, while a poorly-balanced one can create or worsen health problems. We first talked about the microbiome in Episode 9 with Jessica Richman, and today we are going to dig deeper into what affects it.
In this episode, we look at how the microbiome and our life choices impact each other. This can relate to how we live, our health, and even how many mosquito bites we get. Research shows that many chronic and gut diseases are related to our microbiome. We also talk about how medical interventions like antibiotics, Cesarean sections, and fecal transplants change our biome.
– Rob Knight
Advances in DNA sequencing have made it possible to look at the microbiomes of huge groups of people. Several large-scale projects, which we’ll discuss today, aim to look at microbiomes of groups or whole countries. It is also easier for individuals to learn about their own microbiome. This lets you see how your lifestyle, diet, or medical treatments alter your biome.
Today’s guest is Dr. Rob Knight, professor of Pediatrics and Computer Science & Engineering at the University of California San Diego. Dr. Knight was chosen as one of 50 HHMI Early Career Scientists in 2009. He is also a member of the Steering Committee of the Earth Microbiome Project, and a co-founder of the American Gut Project.
Dr. Knight and the Knight Lab at UC San Diego use state of the art computation and bioinformatics to understand the microbiome and what affects it. Dr. Knight is on the forefront of this exciting research and will walk us through the topic.
The episode highlights, biomarkers, and links to the apps, devices and labs and everything else mentioned are below. Enjoy the show and let me know what you think in the comments!
What You’ll Learn
- What DNA and RNA are (6:52).
- Initially researchers thought that the human microbiome would be uninteresting (8:20).
- Advances in DNA sequencing made projects like Human Microbiome Project and American Gut possible (9:53).
- Novel information on how lifestyle affects the microbiome (13:50).
- The different biomes of your body, what is known about them, and how the affect the body (16:50).
- Long-term diet has the largest impact on your gut microbiome (19:40).
- Individuals show variation in their microbiome from day to day, and this variation could make single samples less useful (20:05).
- Research shows that only a few activities and dietary changes significantly affect the microbiome (22:50).
- There are still questions about how variation within an individual’s microbiome relates to health (26:08).
- Resources like American Gut can be used to assess your own response to medical interventions like antibiotics (27:20).
- Fecal transplants to replenish your microbiome after medical intervention is an area of promise for those battling C. difficile (28:15).
- The effect of antibiotics on the microbiome vary among treatments and individuals (31:06).
- The microbiome is incredibly complex, but research into a few microbes could yield tremendous health benefits (33:16).
- Although there is anecdotal evidence that probiotics are effective at positively impacting your microbiome post-antibiotics, there are currently no clinical trials on their effectiveness (37:44).
- The Ancestral Microbiome Project is comparing the microbiomes of people with traditional lifestyles to see if the Western lifestyle or diet has led to a loss of certain microbes (41:05).
- Living with a group of people or a new partner can change your microbiome (42:54).
- IBS has been linked to the microbiome, and probiotics have shown promise for treating the condition (44:20).
- Damien and Dr. Knight discuss places to find additional information on the microbiome (45:22).
- Dr. Knight suggests tracking travel, medications, and diet if you are interested in how your lifestyle affects your microbiome (47:11).
- Those interested in learning more could also track their fitness, do an EEG of brain activity, or an MRI of areas of interest (49:44).
Thank Dr. Rob Knight on Twitter for this interview.
Click Here to let him know you enjoyed the show!
Dr. Rob Knight
- Knight Lab: The Knight Lab is Rob Knight’s laboratory at UCSD. Their research focuses on computational and experimental techniques to ask questions about the evolution of the composition of biomolecules, genomes, and communities, including the microbial ecosystems of the human body.
- Microbes en masse: Nature article on Dr. Knight’s research.
- PubMed Search for Rob Knight.
- Google Scholar search for Rob Knight
- Dr. Knight’s TED talk: How Microbes Make Us Who We Are.
- Crowdfunding site for Ancestral Microbiome Project: Collection of microbiome samples from the Hadza tribe in Tanzania.
- Crowdfunding site for the Human Food Project: Information on donating to several projects.
- Reach the Knight Lab on Twitter
Tools & Tactics
Interventions
- Fecal transplant: The purpose of this treatment is to re-balance the microbiome of the transplant recipient by placing fecal matter from the donor is placed in the colon of the recipient. The most common reason for this treatment is a serious illness caused by Clostridium difficile after the healthy gut microbiome is destroyed by antibiotics.
Supplementation
- Probiotics: Probiotics are live bacteria and yeasts that assist in gut health; this includes antibiotic-related diarrhea, IBS, and IBD. They can be found in a variety of food products (like yogurt with “live cultures”) and in capsule form. Strains of Lactobacillus and Bifidobacterium are the most commonly available.
Diet & Nutrition
- Plant-based diet: Dietary changes can quickly alter the gut microbiome, and Dr. Knight specifically discussed the choice of animal vs plant-based diets on the rates of Prevotella and Bacteroides. Here is the paper by Gary Wu and others discussed Rob Knight. For more information, here is a paper discussing how people on animal-based diets had higher levels of microorganisms related to inflammatory bowel disease in their microbiome.
Tracking
Biomarkers
- Microbiome community composition: To determine what is in your microbiome, labs report the percent of each type of bacteria present in your sample. We are still learning about how microbiomes affect health, so there is currently no information on what an “ideal” microbiome looks like.
- Gut microbiome: This is the microbiome in your colon and is the most commonly assessed of the biomes. Some “good” bacteria like Akkermansia, Lactobacillus, and Faecalibacterium are associated with reduced obesity rates and gut health.
- Fine grade fitness information: This biomarker includes daily information on caloric intake, steps taken, calories burned, sleep quantity, and sleep quality.
- Blood and Urine Metabolites: These small molecules include amino acids, sugars, and fats. They provide insights into health, disease risks, and optimal diet. No specific biomarkers were discussed – the biomarker would be a specific metabolite. A common test is the blood metabolite panel (BMP), which looks at calcium, glucose, electrolyte, blood urea nitrogen, and creatinine levels. For urine, proteins, leukocyte esterase, and hemoglobin are all commonly assessed biomarkers.
Lab Tests, Devices and Apps
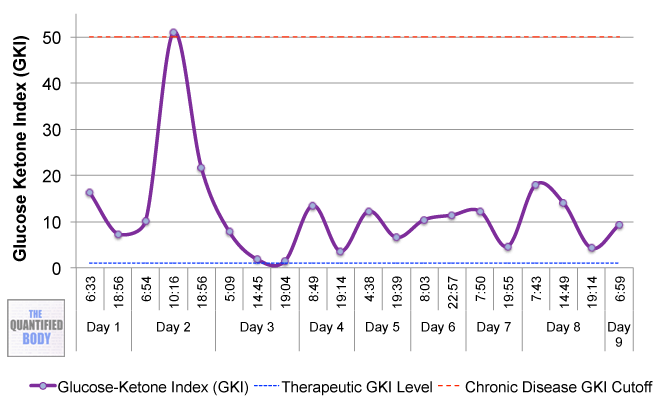
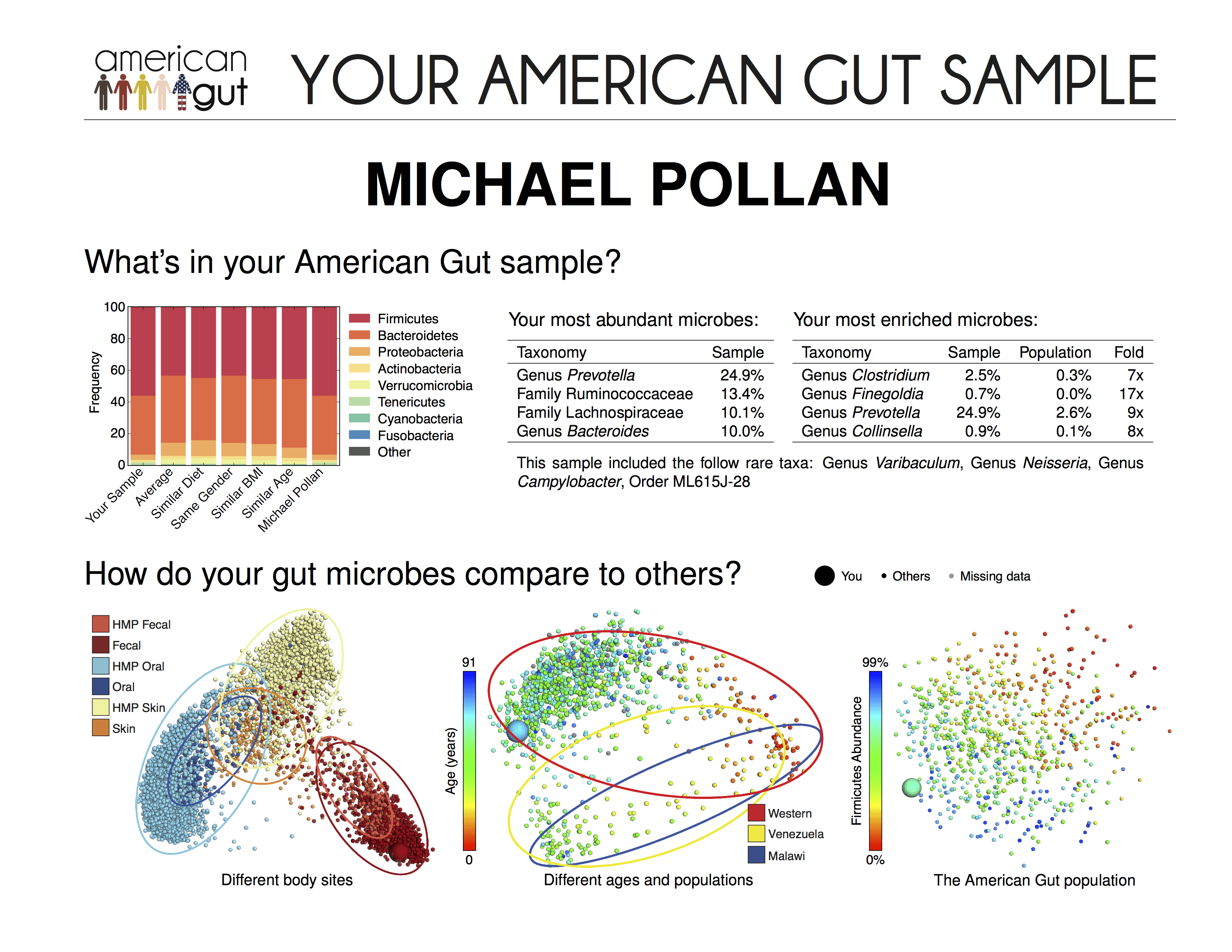
- American Gut Project: A not for profit, research-based initiative to understand the American microbiome. Participants are asked to provide details about their diet and lifestyle.
- uBiome: This test can be ordered and used by anyone in their home. The test allows collection of microbes from your gut, mouth, ears, nose, or genitals.
- Electroencephalogram (EEG): EEGs record electrical activity in the brain. The frequency of waves can indicate whether brain function is normal or disturbed. Alpha (8-13 waves per second) and beta (more than 13 waves per second) waves are the most common in healthy, awake adults.
- Magnetic Resonance Imaging (MRI): MRI scans are use pulses of magnetic energy to visualize internal organs and structures. It can be used on almost any area of the body and provides information on tumors, bleeding, injuries, blood vessels, or infection.
Dr. Knight’s Recommended Resources to Learn More About Microbiome
- Follow Your Gut: The Enormous Impact of Tiny Microbes: Our guest’s book on how the microbiome affects our health. The Appendix includes information on how to interpret the results from American Gut.
- Missing Microbes: Our guest recommended Martin Blaser’s book as a resource for those interested in learning more about microbiomes and antibiotics.
- Not Exactly Rocket Science: A science blog written by Ed Yong, our guest suggested the posts on microbiomes as fun reading for those interested in the topic.
- Some of My Best Friends are Germs: Written by Michael Pollen for NY Times in 2012, the article is a quick read on the relationship between microbiomes and health.
- Jonathan Eisen’s TED talk: Dr. Eisen’s talk “Meet Your Microbes” focuses on microbes and their co-evolution with their hosts.
- Jessica Green’s TED talks: Dr. Green is the founder of Biology and the Built Environment (BioBE) Center, and has given two TED talks on microbes.
- NY Times Matter Column: A weekly science column written by Carl Zimmer.
Other People, Books & Resources
People
- Jeff Leach: Co-founder of the American Gut Project, and microbiome researcher.
- Dr Catherine Lozupone: Professor of Biomedical Informatics andPersonalized Medicine at the University of Colorado, Denver. Dr. Lozupone researchers the impact of the gut microbiome on human health.
- Dr. Jeffery I. Gordon: A research scientist studying the link between gut microbiota and obesity. Our guest collaborated with Dr. Gordon on this topic.
- Dr. Pieter Dorrestein: A professor working at UC San Diego, Dr. Dorrenstein and our guest have collaborated on research. A recent paper of Dr. Dorrestein’s in PNAS looks at the chemical makeup of skin surface and relates it to the microbes that live in the skin.
- Dr. Dan Littman: Professor of Molecular Immunology at NYU School of Medicine, Dr. Littman studies the human immune system.
- Hans Herfarth, MD, PhD: Dr. Herfarth is a member of the UNC Multidisciplinary Center for IBD Research and Treatment and the author for the UNC Patient Guide to Inflammatory Bowel Disease (IBD).
- Balfour Sartor, MD: Dr. Sartor is the co-chair of the UNC Multidisciplinary Center for IBD Research and Treatment.
- Dr. Peter Turnbaugh: A professor in the UCSF department of Microbiology and Immunology.
- Dr. Dave Relman: Dr. Relman’s research focuses on the human microbiome.
- Dr. Cecil Lewis: Dr. Lewis studies anthropological genetics, including the evolution and ecology of the human microbiome.
Organizations
- Human Microbiome Project: A large scale NIH funded initiative to characterize the microbiomes of healthy people. The research in this project helped advance the DNA sequencing tools available today.
- University of Colorado Boulder: Our guest’s former institution.
- The Crohn’s and Colitis Foundation: A non-profit dedicated to finding cures for Crohn’s Disease and ulcerative colitis.
- American Gastroenterological Association: An organization focused on the science, practice, and advancement of gastroenterology.
- Ancestral Microbiome Project: Information on the Ancestral Microbiome Project, a study focused on the microbiome of peoples living in traditional conditions.
Other
- Structure, Function and Diversity of the Healthy Human Microbiome: A paper from the Human Microbiome Consortium on the results of their work. They looked at the microbiomes at multiple body sites of 242 healthy people.
- Rapid evolutionary innovation during an Archaean genetic expansion: A paper by Drs. David Lawrence and Eric Alm reconstructing ancient microbial genomes and their relation to modern day genomes.
- Long-term diet and the gut microbiome: A 2011 paper from Science by Gary Wu and others showing that long-term diet influence the gut microbiome.
- Temporal variability is a personalized feature of the human microbiome: A collaboration by our guest looking at how much variation in there is in an individual’s microbiome over time.
- Affect of antibiotics on the microbiota: A paper by Drs. Relman and Dethlefsen titled “Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation.”
Full Interview Transcript
[05:22][Damien Blenkinsopp]: Hi Rob, thank you so much for joining us on the show.
[Rob Knight]: Sure, thanks Damien, and thanks to your interest on this topic.
[Damien Blenkinsopp]: It’s great. So we’ve already looked at the microbiome, but I wanted to know, why is it that you got interested in this specific area? What is it that first caught your interest, or you first got involved in this area?
[Rob Knight]: Yeah, well it was a very indirect pathway from my graduate work at Predison’s Lab in studying the evolution of the genetic codes and a large part of that was looking at RNA molecules down to particular molecules that are useful in metabolism. So from there I went to the University of Colorado working on RNA sequence states and trying to figure out how many random RNA sequences you need to look at before you find one that does something interesting.
So there were a lot of one particular kind of sequence, the ribosomal RNA molecules in the database. I really wondered why were there so many of that particular sequence that had been studied. And so I started talking to Norm Pace, who was one of the other faculty members at Boulder. And I realized they were using the ribosome’s RNA not as an object of study in and of itself, but as a tool to understand the relationships between different organisms, and to read the mass in the communities that they were looking at. Everything from rocks to shower curtains to caves.
And so it really is just going from basic studies of RNA to understanding that you could use a particular kind of RNA as a tool to find out something about microbes, and then from there realizing that the microbial communities themselves could be used as a tool to find out about different environmental conditions, including the conditions within our own bodies.
[Damien Blenkinsopp]: Great, great, thank you.
[06:52] For some of the people at home, they might not understand what RNA is in reference to DNA, and how that works. Could you give a quick overview of what the mechanism for RNA is, and what role it plays in our bodies and the other things that you’ve been talking about.
[Rob Knight]: Sure, absolutely. So I think everyone’s familiar with the idea that DNA is the genetic material we use that passes down from one generation to the next. So, the proteins are most of the catalysts that do reactions in our bodies, most of the structural elements. So what happens is the DNA gets transcribed into RNA, ribonucleic acid, which is chemically relatively similar to DNA. And then the RNA gets translated into proteins.
But there are some kinds of RNA that don’t get translated, and have a function that is of themselves. One really important kind of RNA is ribosomal RNA that actually makes up the factory in the cell, the ribosome, that makes the proteins. And so because it plays such an important role in life, you can detect similarities in those even between very distantly related organisms.
So similarities even between us and bacteria. And so you can use that molecule to reconstruct the evolutionary tree that relates all of those organisms together, based on the similarities and differences in the sequence.
[08:04][Damien Blenkinsopp]: Great. So then you, from those studies, you started working to look at the bacteria, because you saw that they had a pretty important role, and that there was a lot of similarities between the things you were studying. On a human level and in the animal level, could you tell us a little bit about what it was that kind of pushed you to look more at the microbiome?
[Rob Knight]: Yeah, sure.
Originally the tools that I was developing together with Cathy Lozupone, then a very talented graduate student from my lab but now a faculty member of the University of Colorado Health Science in Denver. Initially we were just looking at tools to compare microbial communities out there in the environment.
So looking at the effects of things like salinity and pH as the chemical factors, of drivers, for how microbes are different in different places, like different samples of soil, sea water, or other communities like that. And so at the time we thought that maybe the microbes associated with the body wouldn’t be that interesting, because at the time there was fairly heavy bias towards the idea that most people probably have the same microbes, because if you grow them on a Petri dish, you get more or less the same thing from everybody.
But it turns out there’s a huge number of microbes in there, even in our own bodies, that we don’t yet know how to culture. And as a result, when you look at them with these culture independent, they are directly sequencing the DNA that codes these ribosomal RNA genes. And figuring out what’s in the communities directly you see all this diversity in the human microbiome that no one ever suspected was there.
So, we started doing this in mice, actually, in collaboration with Dr. Jeffery I. Gordon, he’s a physician at Washington University, a gastroenterologist. He was really interested in looking at links between microbes in obesity. So we started with mice, then moved up to humans. And then increasingly we’ve been interested in looking at the microbiome not as a static system, but as a dynamic system. So looking at how it changes over time, both in health and in disease.
[09:53][Damien Blenkinsopp]: Great, great. Thank you very much. And of course you are a co-founder of a project, which is being designed to explore the microbiome in America, of the population in America. What kind of latest update of American Gut, and what you’ve been doing there?
[Rob Knight]: Let me give you just a little back-story to that project. So, before American Gut, we were involved in the Human Microbiome Project, which was a very large scale NIH funded initiative, 173 million dollars to characterize what the microbes look like in healthy people. And with their whole microbiome, is there a lot of variation person to person, and how does it vary in different parts of the body.
So during that process, and in part because of technology that was developed, during the Human Microbiome Project DNA sequencing and tools to analyze the DNA sequences made the whole process dramatically cheaper. So essentially we wondered can we bring this technology to members of the general public, using the tools that we were able to develop during the Human Microbiome Project, to essentially allow anyone who was interested in finding out about their own microbiomes to be able to do that at a reasonable cost.
Jeff Leach and I launched as a collaboration between the Earth Microbiome Project and the Human Food Project. The crowd funded initiative where basically it’s donation supporters. And people can find out directly about swabs from their gut, and how it compares to the gut microbes of other people around America, or around the world, especially including the people who were analyzed in the Human Microbiome Project.
And also including people in Africa and South America, and soon people in Asia, to try to compare what the microbes look like, and how do they relate to health and disease.
So, unlike the Human Microbiome Project, where there were very rigorous exclusion criteria, so you could only participate if you were certified by a physician as being extremely healthy, in American Gut, we are interested in anyone, essentially to see what kinds of microbiome configurations are out there in the wild when you give everybody the opportunity to participate.
[Damien Blenkinsopp]: Great, great. That’s a great back-story.
[11:54] What’s the number of samples that you’ve collected to date? You said it’s called American Gut, but it sounds like it’s not just focused on America now, that it’s spread out and it’s available to more widely internationally. Is that correct?
[Rob Knight]: Yeah, that’s correct. So it’s relatively expensive to pass inspection internationally because the shipping regulations are fairly burdensome. So what we’ve been doing is we’ve been launching spin-offs in other countries. And so we started with Australian Gut, and with British Gut essentially because it’s a lot easier to translate all the instructions from English into English, rather than to tackle those translation issues.
But we’re hoping to expand to a lot of other countries. And at the moment with the transition from the University of Colorado to the University of California, we’re essentially in a holding path, and at the moment waiting for AMX approval. But we’re hoping to scale up the project dramatically, and greatly facilitate the ability for people all over the world to participate.
[Damien Blenkinsopp]: Which approval did you say you were waiting for? Was it an academic program approval?
[Rob Knight]: Institutional Review Board Approval. So in order to ensure that the project was conducted ethically and that the results that we get are going to be meaningful, everything we do in American Gut has been approved by Institutional Review Boards from the beginning.
I moved from the University of Colorado to the University of California right at the beginning of this year. What’s happening right at the moment is we’re waiting for the ethics approvals to be transferred from one institution to another, which can take a lot of time.
[Damien Blenkinsopp]: Right, right. Got it.
[13:19] How many samples have you collected to date for the project?
[Rob Knight]: We’ve released data from about 4500 samples. We’ve sent out about 9,000 kits. We have about another 1500 samples in hand that we’re just waiting for that ethics approval to be able to move forward on sequencing.
So, for anyone who’s listening, if you’re wondering where your results are, we’ll be able to get them out pretty soon. We just need to make sure that everything is completely compliant with all the regulations that apply to the Human Subject Research in the United States. Just to make sure that everything is completely above board.
[Damien Blenkinsopp]: Excellent. So, has any analysis come out of it, or insights yet that you’ve been able to do?
[Rob Knight]: Yeah, absolutely. So one thing that was exciting about it, or already, in the Human Microbiome Project, this paper, which came out in Nature in 2012, we looked at about 250 healthy subjects. So I think we reported data for 242 where there was information from all body sites.
So you have about 250 people involved in that project. Versus American Gut, where you have thousands of people involved. As a result, with a much larger population size we have much more statistical power to look at subtle effects.
And we also put on the questionnaire all sorts of things that were considered too crazy to ask in the HMP. But in the intervening time we’ve discovered so much more about what the microbiome does, especially in a range of different animal models. And it seemed a lot less crazy to ask those questions in 2012 than it did in 2008.
As a result, we’ve been able to see associations between the microbiome, and all kinds of things you might not have expected. So you might have expected that how old you are affects the microbiome, which it does, but you might not have expected that, for example, how much sleep you say you get a night is also linked to the microbiome. And we see a statistically significant effect of that.
Similarly, you might have expected that how much alcohol you drink affects the microbiome, but you might not have expected that we can also pick up a difference based on how much you exercise. Or I should say how much you say you exercise, because all of this is reported data. But how much you say you exercise, even whether you say you do it indoors or outdoors, has an effect.
So we’re really picking up a lot of interesting associations. And what we’re hoping to do in the next stage of the project is to take a bunch of these associations and turn them into something where we can start to get causality. So what we’d love to know, if we see in association with alcohol and an association with exercise, or with sleep or with any of these other things, is to actually encourage people to change what they’re doing in those respects, or you know more obvious things like diet, or antibiotics.
Where the idea is that if you take a sample before you have a change in any of those things, and then you have the change and then you take another sample again after. Can we start figuring out which of those changes are actually caused by those different lifestyle things that you could be doing. This is watching simply effect.
[Damien Blenkinsopp]: Right, because a lot of when we’re thinking about the microbiome, and –just to make sure I’m correct here — you’re just looking at the gut, right? The microbiome of the gut?
[Rob Knight]: Well, actually with American Gut you can look at the microbiome. So most people are looking at their gut biome, but it’s also interesting to look at other body sites. We have been sending out a number of batches of kits that allow you to sample multiple sites simultaneously.
So another project we’re doing, we’ve been looking at skin. So for example, we had a very interesting paper that came out in PNE of last week with Pieter Dorrestein doing very high resolution maps of the skin in relation to the microbes, to the metabolites. And then there’s also a lot of interest in the oral microbiome, the vaginal microbiome, and so on.
So, although the gut microbiome is where most attention has been focused, there is a lot of interest potentially in looking at other body sites. And linking them not just to health effects of that site, but also to all over the body. So for example the gut microbiome has been linked to asthma and to rheumatoid arthritis, and to cardiovascular disease, all of which takes place in sites outside the gut, but are nonetheless affected by the microbiome.
And it’s entirely possible that, for example, the oral microbiome, or the skin microbiome might also be having systemic effects we’re only just beginning to understand. Whether it’s through interactions with the immune system or through release of particular metabolites, or other mechanisms.
[17:32][Damien Blenkinsopp]: Maybe it’s too early to say this, but have you seen anything that would indicate that the microbiomes are related to each other, in terms of if you have a different gut microbiome it may influence or be influenced somehow by the fact that your nose or your skin biome is different also?
[Rob Knight]: Well that’s a very interesting and controversial question. So actually, the fifth Human Microbiome Project main papers, which said that there are statistically significant but relatively weak associations between the different body sites, and then later that’s been confirmed by other researchers using different statistical methods.
At the moment there’s a lot of debate about how strong the associations are, and what effects they have on health when you’re looking at the overall configurations. But certainly some individual organisms that are very interesting. So, for example, Dan Littman at NYU has shown some very nice work linking Prevotella in the guts to rheumatoid arthritis. And so we’ll probably see a number of other associations like that with specific organisms at one site having unlikely effects on what happens, what helps with other sites in the body.
[Damien Blenkinsopp]: Very, very interesting.
I think the surprising thing for a lot of people of what you just said is that there are a lot of lifestyle factors not related to diet. Because we normally think of the biome, and especially the gut biome, being immediately related to our diet, and what do we eat, but [not] a lot of things you mentioned, sleep, age, exercise. And you said exercise indoors or outdoors can be different as well, is that correct?
[Rob Knight]: Correct, yeah.
[Damien Blenkinsopp]: So you know, it’s very interesting. These small changes in your lifestyle, nothing to do with diet, can have significant impact on the gut also, which we haven’t looked at.
[Rob Knight]: Sure, although I should clarify that long term diet has the largest effect that we’ve seen. The work with Gary Wu and others at Penn came out in 2011 in Science. What we saw there is this long-term dietary pattern had a profound effect on the gut microbiome, especially changing the ratio of Prevotella to Bacteroides, two of the major taxa in the gut. And only changing the overall configuration, more than essentially anything else.
So the only thing we’ve seen that gives you comparable changes is either antibiotics or acute infection with some kinds of pathogens. Like C. diff, for example, has a very large effect on your gut microbial community. So long term diet is really very important.
Short term diets, unless it’s something really extreme, is a lot less important than what we see in long term diet. This was maybe consistent with people’s experiences with going on a diet for a short period, losing some weight, but then going off the diet and bouncing back again. In general your microbiome is very resilient.
[20:05]Damien Blenkinsopp]: This comes to the topic of variability of the microbiome over time.
I did see one presentation of yours where you were showing the biome of a newborn baby, actually, as it was growing up. And you’re showing the changes at that stage of its life, which were quite significant at that stage. But for adults who are fully developed, in our day to day, week to week lives, are our microbiomes changing significantly? Or are they very, very stable?
[Rob Knight]: Both of those are true. So, our microbiomes change statistically significantly one day to the next. And especially when we do things like travel or take antibiotics, or if we have a chronic, immunologically associated disease. Like, for example, inflammatory bowel disease, or rheumatoid arthritis, or other conditions where there’s a lot of variability in whether you’re in remission or whether you’re having a relapse.
There can be fairly large changes there, but typically small compared to the differences between different people. So we tend to be stable in terms of, especially if we’re healthy and there’s nothing particular going on, we tend to be stable in the sense that we’re more similar to ourselves day to day than we are to other people.
But that doesn’t mean that you can’t detect the differences one day to the next. And so a very interesting question at the moment is what is the significant of those day to day fluctuations? Might it actually be more important how much you vary than what your current state is right now. And that’s one of the things that we’re just starting to investigate at the moment.
[21:29][Damien Blenkinsopp]: Yes, and in terms of how meaningful data would be for someone who’s collecting it for themselves, if they take one sample and they get one reading is that meaningful to them? Or would you suggest they take one this week, and one next week. How would you go about making sure you have something representative?
[Rob Knight]: Right. Well having one sample is certainly a lot better than having no samples, in terms of getting some information about what’s in your gut. Because even having one sample is going to do a tremendous amount to place yourself on the microbial map, relative to other people.
The question about how frequently you should sample and how many samples you should take to get a baseline, that’s something that’s actually a very active research topic at the moment. And we have collaborations with a number of different investigators exploring that in different contexts.
So, for example, one thing we’ve been doing is work supported by the Crohn’s & Colitis Foundation of America with Hans Herfarth and Balfour Sartor of the University of North Carolina, where we’re trying to address exactly that clinical question. If you have patients with IBD should you sample daily, should you sample weekly. So how does that compare to what you should do in healthy controls.
Unfortunately, the only way we can assess that baseline data is to take very frequent samples. And it’s difficult to get people to do that. So for example, I’ve been collecting my own samples daily for over six years now. It’s relatively difficult to get people to come up to that kind of level of commitment.
[22:50][Damien Blenkinsopp]: So, I’m interested. What kind of insights have you learned about yourself from that n=1?
[Rob Knight]: As you know it’s always relatively difficult to draw conclusions from a sample size of one, but it does look like things like travel have a fairly large effect. We’ve seen that for a number of different locations.
So I should clarify that only about the first two years of that have been sequenced so far. Most of the rest are in a queue for processing, but it keeps getting bumped due to things like making sure we get the American Gut results and so on. The rest of the time series is currently pending.
We’ve done the DNA extraction so that’s currently pending sequencing. And some of the things that we’re going to be really interested to follow up on, having a time series that goes that long is, for example, the seasonality effects that we seen in American Gut. And we see those even within one individual. Because if you can repeat that for many years, then you can start to see systematic patterns.
I’ll tell you about some results from another study, which is one by Lawrence David and Eric Alm at MIT, where they sampled themselves daily for a year and collected a very large number of auxiliary variables. I think they collected over 100 variables every day, including everything they ate. All kinds of things like how much exercise they did, how much they slept, and so on.
And they found very few systematic associations. So, for example, about the only thing they saw in diet was citrus, which had a significant effect, whereas many other things that they recorded did not. And they also saw associations with travel, and associations with getting GI illnesses. And that was about it.
So, I think the issue is that a lot of the effects, although they might be important, they’re probably subtle and cumulative. And so although you’re going to get very interesting information from some of these n=1 studies, like this study. And by Larry Snar here at UCSD has been doing looking at his own gut in the context of IBD, in the context of my studies myself.
Although there’s going to be some interesting stories that come out of them, those are going to be most interesting in terms of the technology development, of asking how frequently should you sample to establish a baseline, and over what interval to you need to sample to get a decent view of dynamics.
But we did a study with Noah Fierer and Rob Dunn, Greg Caporaso that came out in Genome Biology towards the end of last year looking in healthy students at the variation of the gut microbiome over the course of the semester. One thing that was very interesting about that, looking at weekly samples, was the variability itself seemed to be very important for relating to the variables that we had about each subject, and each sample.
And so it’s entirely possible that the variability itself was going to wind up being really important. But of course, it’s also a lot more difficult and a lot more expensive to look at than just looking at a single snapshot. And so the single snapshots are still very valuable, I meant to say, even though you could potentially get more information by looking at the dynamics than you would from a single snapshot.
It’s like having a video of an event can often be very informative, but that doesn’t mean that photography has vanished as a discipline despite the fact that we all carry around little video cameras on our cellphones.
[26:08] [Damien Blenkinsopp]: Great.
So in terms of the variability, is it looking that that’s a positive or a negative association? Maybe you can’t really call it yet, but have you got an idea on which way it would be going? Like, for instance, is it potentially that the microbiomes when it’s healthy it’s able to adapt a lot more to the day to day situation, travel and all those things, so it would vary more. Or have you got any insight on that yet, or ideas on which way it might go?
[Rob Knight]: Yes.
So we don’t really have enough information at this point, and as you say it could go either way. Either you might want to see a fair amount of flexibility in your microbiome to be able to adapt to different circumstances, or you might want to see more resilience, and if it’s wandering all over the place it’s more likely to fall off a cliff, and to input the community configuration.
Right now we don’t have the basis to discriminate between those two. Most of the variability studies have been done at baseline in healthy people, and that doesn’t necessarily let you conclude anything about disease.
Most of the disease studies have looked at a relatively small number of samples. Often just a single sample where you’re looking at a case controlled paradigm where you round up some healthy people, round up some sick people, and you look at the differences at that state. So, really we’re waiting for the right kinds of studies to be done for variability in these diseased populations.
[Damien Blenkinsopp]: Great, thank you very much. I mean, we could get a couple of guidelines, just for people who are already using American Gut or one of the other services.
[27:26] I’m actually just about to take some antibiotics, for instance, so I’ve got a kit I intend to use, and then once the course is finished I intend to use it again. And actually based on your presentation, I intend to do one 30 days later to see if it will recover. Is that something reasonable as a baseline experiment? Just to see what’s going on.
[Rob Knight]: Yeah, that’s certainly very reasonable.
You might want to look at Dave Relman’s paper, it came out in Pathobiology a few years ago. And what he had there was three subjects who were taking ciprofloxacin from a healthy baseline, and they measured how long it took them to come back.
What was interesting about that is three people, they all responded totally differently. But then it’s kind of difficult to figure out what you should say about that, because the sample size is only three, and they all responded very differently from one another. But it’s certainly reasonable.
One thing that’s very interesting at the moment is the concept that maybe you should freeze your stool before you take the antibiotics, so that you could potentially replenish the members of your community. And again I should point out that that’s still in its very early stages as a therapy. This is not medical advice or anything.
But the concept that you might want to have that material available in case we figure out how to replenish your microbes from it later, kind of the way people are saving their cold blood for the stem cells. It’s certainly very interesting, and has a lot of potential.
And of course, right, you’ll be hoping for is that in the relatively near future – and there’s a lot of companies and a lot of academic research groups interested in this now – the idea that you might not actually have to take the stool itself, but rather isolate just a few of the beneficial microbes from it, encapsulate those into a pill and swallow those, for example. That’s shaping up to some very interesting research direction, although at this point it is very much in the lab and not in the clinic.
[Damien Blenkinsopp]: It does sound safer, also compared to the current fecal transplants. I think one of the concerns of fecal transplants is we don’t really know what’s in them.
[Rob Knight]: Yeah, that’s exactly it.
[Damien Blenkinsopp]: You know, because just the state of technologically today.
While you might make someone better in some extreme cases, like C. difficile, obviously that’s helpful. But for someone else who has maybe taken a lot of antibiotics and they had gut issues, to take a fecal transplant could be seen as a little bit extreme, as currently we’re not exactly sure what’s in it, and we could be putting something in there that we’ll discover later is not such a good thing.
[Rob Knight]: Yes, that’s certainly a concern. I’m on the science advisory board for the American Gastroenterological Association’s Microbiome Center, and one thing we’re actively trying to set up is a long term registry for fecal microbiome transplant, essentially so that we can track people who’ve had them over time, and make sure that it remains effective.
So for Clostridium difficile associated disease, it’s remarkable effective. Like 90 to 95 percent effective in many different studies. And the last large scale study comparing it to antibiotics for C. diff actually had to be stopped early because the people who got the FMT were responding so well that it was unethical to continue withholding FMT from the people who were on the antibiotics.
So, how widely that’s going to work for other conditions, we don’t really know. One thing you can do for antibiotic associated diarrhea that’s very effective is probiotics. There’s a number of different ones that are now pretty well supported by clinical trials at reducing both the severity and duration of antibiotic diarrhea.
And so in general, it’s not because the organisms themselves are establishing in your gut, but they’re creative a favorable environment where they can crowd out the weeds, like the proteobacteria and things that often come back after antibiotics. And essentially they’re creating more favorable conditions for your own microbes to come back.
[Damien Blenkinsopp]: Great.
[31:06] So, to kind of backtrack a bit. So in the presentation I saw, you saw after the antibiotic treatment, which was a baby with earache I believe it was, the microbiome pretty much came back to where it was before.
[Rob Knight]: Yup. But remember that’s an n=1 study, because we just had one kid in there. Yup.
[Damien Blenkinsopp]: So is that a possibility for some? We always talk about antibiotics like it could be potentially permanent. Because everyone’s pretty concerned. I’m pretty concerned when I’m going on a course of antibiotics now what kind of impact down the line is it going to have.
But it seems like it can depend on the severity, because antibiotics are used in many different cases. They can be used for a couple of days in some cases, sometimes, and there’s lots of different forms of antibiotics, which have different impacts as well, and potentially more severe or less severe.
It seems that in some cases the microbiome may be able to recover, and in other cases it’s not able to fully recover, and it’s quite variable for the moment, I’m guessing. Or do you have any insights as to the insights of antibiotics and how it varies?
[Rob Knight]: Basically what we know at this point is that different antibiotics have very different specificities, so they’ll target different bugs when they’re growing in the lab in isolation. We know a lot less about what effects the antibiotics have in more complex settings. And so the same microbe might only be targeted by antibiotics in some stages in it’s growth cycle.
And so Pete Turnbaugh, he’s now at UCSF but did this work while he was at Harvard, did some very interesting research looking at the effects of the same antibiotics microbes in different communities, that had come from different individual people. And so what he found is even if you have the same microbe, whether the same antibiotics would target that microbe depends a lot on who it came from.
And that’s very interesting. It just suggests that there’s a lot of complexity that we don’t understand at this point about how microbes are going to be targeted by a particular antibiotic, or will escape that depending on what other microbes are around. Depending on whether it’s expanding its population or contracting it, and all kinds of other factors.
So I think we’re just right at the beginning of understanding what’s going on in the complex situation of the human body itself.
[Damien Blenkinsopp]: Yes, absolutely.
[33:16] I think a bit of context to that is if you look at the size of DNA in our genetics versus the microbiome, right the microbiome is a lot bigger, and we don’t fully understand DNA yet. So, basically is it a much bigger task to understand the microbiome?
[Rob Knight]: Yes, it’s a tremendously more complex task. So each of us has about 20,000 human genes, but the size of the microbial gene catalog is somewhere between 2 and 20 million. So, by that measure you could say that we’re only about one percent human, and about 99 percent microbial in terms of the gene counts that we’re carrying around with us.
And so, on the one hand understanding it is tremendously complicated. On the other hand, if you look at other fields where there’s tremendous complexity, like say nutrition for example, but if you ran a potato through the mass spec you’d see all these compounds that you’ve never seen before, and that you don’t understand, and that don’t appear in any catalog from any chemical company. On the other hand, that doesn’t mean that we don’t know a fair amount about what happens if you rely on potatoes as your main food source.
And additionally, if you look at, for example, a lot of chronic diseases from a century ago, so things like rickets, goiters, and so on. A lot of those kind of diseases have just been completely eliminated by knowing that there’s some nutrient that if you give it to the whole population, like for example iodine in salts or fortifying milk with vitamin D, fortifying flour with thiamin, and so on, you can just eradicate these diseases from the whole population.
And so, in the same way it’s going to take us a long time to understand the microbiome, but it might not take that long before we understand how replenishing some of these microbes might potentially be really important for addressing some of the chronic diseases that affect us now, including many of the chronic diseases still linked to the immune system.
[35:11][Damien Blenkinsopp]: Great, great. And there are also macro levels. It’s a pretty good example, I think, you just gave nutrition, because we look at the macros and there’s lots of discussions about proteins, fat, and carbohydrate breakdown in diets. And in the same way there’s macro levels of our microbiome, right? There’s groups of Firmicutes and Bacteroidetes and others on a macro level, which I guess you could see patterns with those as well, and don’t necessarily have to dig down to the fine levels.
[Rob Knight]: Yes. That’s exactly right. Although in the same way that micronutrients are really important, some of the rare organisms might be really important.
And a useful analogy is something like Yellowstone National Park, where the reintroduction of wolves caused a profound change to the ecosystem. But if you go to the park – and not without, but you’d never get permission to do this right – but if you went to the park, and you round up say a cubic kilometer of material and then run that through DNA sequencing, you wouldn’t find a lot of wolf DNA.
And the reason why we know their important is you know people shot them all and the ecosystem changed, and they reintroduced them and the ecosystem changed again. So on the one hand, what technology is that we have right now, we’re probably missing the equivalent of the microbial wolf that could be playing really important roles.
On the other hand, if you were trying to understand that ecosystem, you’d be crazy to ignore the pine trees and the bison and the other really abundant taxa as well. So you can tell a lot looking at what’s common as well as needing to know what’s rare to fully understand the system. But I think we’ll be able to do a lot with the understand that we have now.
And it’s important to remember that that understanding has increased dramatically just in the last decade. So in 2005 it was a major achievement to sequence the gut microbial communities out of three people. And that was expanded by a fifth to hundreds of people, and then to thousands of people. And we’re just getting a much broader picture of what kind of microbes are in there, and what their roles are in responding to different things.
And so, the idea that you might be able to look at the microbes in somebody every single day for a year, would have been an impossible dream in 2005 but the technology has gotten so much better that it’s been done for a number of people now. And the prospects for developing further technology to open that up to the whole population I think will totally transform what we can know about microbial sides of yourself.
So, being able to push that additional technology development forward I think is one of the most critical things we can do at this point.
[Damien Blenkinsopp]: Excellent, thank you very much.
[37:44] One of the things we kind of skipped over but I thought might be interesting for the audience is you spoke about probiotics being useful in connection with the antibiotics treatment, and specific types of probiotics.
Do you know specifically what those are? Or could you point us to any papers which highlighted those? And in terms of the timing, do you take them while on the antibiotics, or is it a post treatment?
[Rob Knight]: The different studies that have been done at the moment haven’t really had a lot of consistency in methodology, so it’s difficult to make specific recommendations. It’s a fairly complex topic. I cover this in a reasonable amount of detail in my book, Follow Your Guts, which is just coming out tomorrow. But essentially I give a few examples of pointers to studies that have been focused on individual probiotics that have shown to be effective for particular conditions.
So one thing to remember with this is although there’s a tremendous amount of enthusiasm to probiotics and they’re very widely available, most of the specific products don’t have any particular evidence backing them. And so it can be a bit daunting to wade through the literature and try to find the ones that are actually supported by clinical trial data.
At the moment, at least to my knowledge, there’s no really good resource that summarizes the clinical trial information to tell you what species, what strains, and what products containing those strains have actually been shown to be effective. Although that’s something that’s a clear opportunity, where if someone sets it up that will be tremendously valuable for the public, especially given the level of enthusiasm.
One problem at the moment is, in the US at least, that the FDA’s official stance is that a dietary supplement can’t modify a disease endpoint. So as a result, if you find that your product actually does modify a disease endpoint, then it gets re-regulated as a drug, and so the manufacturing standards are certainly much more stringent.
And so if you want your yogurt with live and active cultures to continue to be a buck or two a cup, rather than being a thousand bucks a cap, which is about what it would cost if you had to manufacture it as biologic, there’s that issue to consider as well. So, that’s also a substantial problem for research in this area.
[Damien Blenkinsopp]: Right, so again, in that case we’re kind of hoping that no one tries to do clinical trials with the probiotics in products. It’s kind of no-win situation in that respect.
[Rob Knight]: Well it is a bit of an issue. It’s sort of like the issue with dietary supplements for athletic performance. So any time one tends to actually be effective, like say steroids, for example, it gets banned immediately. So you can draw your own conclusions about the effectiveness of the ones that are still on the market.
[Damien Blenkinsopp]: I guess one of the nicer things about that is currently when we take antibiotics it’s not really acknowledged that it causes any specific disease, although people may have gut upsets and any issues like that.
So I guess if these supplements continued to be marketed, and perhaps trials are just done on the basis of changing microbiome, that wouldn’t interfere because it’s not a disease endpoint. A specific disease endpoint, as I understand it, would be a specific classified disease, which is currently basically regulated today. So as long as they stay out of those disease areas, is it not a problem?
[Rob Knight]: Yeah, that’s exactly right. And that’s in part why as a consumer, it’s often very frustrating to see what claims are being made because those claims are now typically very carefully worded and very carefully negotiated.
[41:05][Damien Blenkinsopp]: So I know that you’re also involved in the Ancestral Microbiome Project.
[Rob Knight]: Uh-huh
[Damien Blenkinsopp]: Could you give us a quick update on how far you’ve got with that, and also what it is for the people at home.
[Rob Knight]: Sure, absolutely.
So the goal of this project is essentially to compare the microbiomes of different people living relatively isolated lifestyles and seeing whether they contain microbes that we as Westerners have lost with the hygiene or antibiotics. Or diets perhaps, that cause us to lose some of those kinds of microbes that could be beneficial.
There was a paper that just came out two weeks ago led by Cecil Lewis at the University of Oklahoma on the Matses who are a group of hunter-gatherers in Peru. There’s another one coming out soon that I can’t tell you about because it’s embargoed. But there’s some ongoing work that we’re doing with the Hadza in Tanzania, and the project that’s led by Jeff Leach.
So the Hadza are the last hunter-gatherers in East Africa in the Rift Valley where, of course, humanity evolved. So they’re the last group that’s still exposed to the microbes and to the mammals and to the plants that we would have evolved with during our early evolution. And so they’re very exciting to look at from that standpoint.
But basically the idea is to compare different groups and to understand first there’s still anything that they have in common that we might have lost more recently. And then the second thing is that try to understand similarities and differences in different human populations in terms of their microbiomes and how those microbes relate to different lifestyle features, to human genetics and to other factors.
It’s going to be incredibly fascinating from a science point of view. And from the point of view trying to figure out how our microbiomes should be shaped to optimize health.
[Damien Blenkinsopp]: Yeah, this is great.
I understand that Jeff — have you spent time with the Hadza as well, or has it just been Jeff that’s spent the time with the tribe?
[Rob Knight]: I went there for a week last year. It was just a spectacular experience.
[Damien Blenkinsopp]: I understand that Jeff, at least just spending time there, his microbiome changed. And he also used a fecal transplant from the Hadza to see a more extreme change.
But what I thought was interesting was just living amongst them and spending time with them, he saw some changes in his microbiome also. But I guess you haven’t had your sequenced yet, but potentially over that week you would have seen the same changes.
[Rob Knight]: Possibly. We don’t have the sequence data for that, although that would certainly be interesting to look at.
I should note that’s also true if you start living with a new partner, for example. You’ll converge on their microbiomes relatively rapidly. And one thing of interest at the moment is trying to figure out how much your microbiome records about the people you’ve lived with and the places that you’ve lived.
We don’t really know the answer to that at this point, but it’s certainly interesting to think about.
[Damien Blenkinsopp]: Well it is, just from a health perspective as well. Especially as it’s getting quite common to have IBS and things like that these days. It kind of makes you question these kind of things. How communicable is it, or not? I guess there’s a lot.
[Rob Knight]: Yeah, that’s a great question. I don’t [think] there’s been done a lot on communicability of IBS, but there are some probiotics that have done pretty well in clinical trials for IBS.
[Damien Blenkinsopp]: Yeah. So we’ve got a solution anyway.
[Rob Knight]: Yeah, and it has been linked to the microbiome by a number of different studies including some work we did with [unclear 44:25]. So yeah, it’s definitely a fascinating area. And the potential that some of these conditions could have microbial cures as well as microbial causes is very interesting.
[Damien Blenkinsopp]: Great, thank you very much Rob.
[44:40] So what are the best ways for people to connect with you, and learn more about you and your work?
[Rob Dunn]: Well, my TED Talk is a really good starting point. There’s a book associated with that Talk called Follow Your Gut, which is going on sale tomorrow actually.
[Damien Blenkinsopp]: Is that on Amazon?
[Rob Knight]: Through Amazon, and also I think it’s available as an iBook through the Apple Store. That’s a good way to find out more. It’s a relatively short book. The idea is to make it a friendly general introduction rather than going into a lot of technical detail about a whole lot of names that you’ve never heard about.
And also it’s got an Appendix that gives you a good overview of how you should interpret your American Gut results, and what things you can and can’t learn at this stage, and what we hope to be able to find out from us in the future.
[Damien Blenkinsopp]: Great, we’ll put links to all those in the show notes.
[45:22] Are there any other good books or presentations for people interested in the microbiome in general, and learning more about it? Are there any references that you commonly give out to people, which are good resources to check out?
[Rob Knight]: Yeah, Marty Blaser’s book. So Marty Blaser’s book Missing Microbes is fantastic, and really gets into a lot of detail about how hygiene and antibiotics may have led to the rise of a lot of autoimmune diseases, and other chronic diseases that are a problem today. And also one specifically about the dangers of over prescription of antibiotics. So I definitely recommend that one.
Ed Yong’s blog, Not Exactly Rocket Science, routinely covers microbiome topics. As do Carl Zimmer’s columns. Michael Pollan wrote a very nice piece in the New York Times in 2012 called “Some of My Best Friends are Germs,” and he’s continued to cover the microbiome on and off since then. Those pieces are all very good.
Jonathan Eisen and Jessica Green both have talks that are available through TED. Jonathan’s talk gives a very good introduction to what microbes are and what they do out there in the world. And Jessica’s features, it’s focused more on the built environment. And it’s talking about the relationship between the microbes in our bodies, and in the spaces we inhabit, and how we might want to design buildings that are green not just in terms of the plants, but also in terms of the microbes. So not just energy, but also microbial use.
So those would be some really good places to start. There’s definitely a lot of more technical resources out there, but you can probably get to those from the ones that I mentioned. And especially the references in Marty’s book and in my book are a good place to get started with more technical material.
[Damien Blenkinsopp]: Great, thank you so much for that. That’s very extensive, clearly.
[47:11] So I’m also interested what your personal approach is to body data, whether it’s for your health, your longevity, or your performance. Do you track and metrics or biomarkers for your own body on a routine basis?
You’ve already said that you take stool samples every single day. Is there anything else you do? And those stool samples, just by the way, for instance if you go to the toilet twice per day, do you take two stool samples, or are you taking one per day?
[Rob Knight]: Initially I was taking one per day, and I’m trying to capture all of them to the extent possible.
So in terms of auxiliary data I must admit that I’m not nearly as diligent as some other people who are interested in this sort of thing have been at tracking every single thing they’re doing every day. In part that’s informed by some of the studies where people have tracked a tremendous number of measures and not seen a lot. So that’s been relatively difficult to justify that level of additional time commitment.
Mostly what I’m tracking are things like, so periodically I’ll do a food and dietary inventory. Tracking things like travel is important. I would track medications except I essentially haven’t had any during that interval. But it’s the sort of thing that I would keep track of if it became relevant. That kind of thing.
[Damien Blenkinsopp]: Great, great. I’m guessing that most of these things are something that you’re doing in the realm of science, because you’re exploring the specific subject.
Do you think you would control for any of these if you weren’t involved in the science itself, out of a personal interest? How would you kind of modify that, if you weren’t currently studying you as an n=1 experiment to further the science? On a personal level, what kind of things do you think you would be doing?
[Rob Knight]: All kinds of things are interesting, it’s just a matter of how much time you’re willing to put into it, and how much money. So it would be very interesting to do blood and urine metabolites frequently, perhaps even daily.
It would be very interesting to get finer grade resolution on fitness, like with an activity tracker, that kind of thing. Given what we’re now starting to find out about brain microbe links it might be really interesting to, for example, track EEG readings over time and draw those microbial data.
You could even imagine doing like an MRI of yourself every day to see whether that complex multifarious specs tracks what the multifarious specs to find biomarker biome. Although that’s definitely a level of efforts and expense that it’s just not worth it at this point.
But what I think this is one of these things where the more data you have, the more potential you have to find out something really interesting that you wouldn’t have expected.
[Damien Blenkinsopp]: Great, thank you so much.
[49:44] The last question, what would be your number one recommendation to someone who is trying to use data in their life for better decisions about their health, their performance, or longevity? Something about their body. What would be your number one recommendation on how to use data effectively?
[Rob Knight]: There are a lot of different ways that could answer that question, but I guess my number one recommendation would be that what’s in the literature, like randomized controlled trials about what works and what doesn’t, are probably a really good guide as to what you should do initially.
Now, you might want to modify that based on observations of your own body, because anything that’s in the literature has got to be based on population averages. And one thing we know about people is that there are tremendous amounts of variability. So what works on average in the clinical trial is not necessarily going to be what works for you individually.
So, start with solid evidence from clinical trials, especially randomized placebo controlled trials, and then modify that based on your own observations about your own health whether it’s meticulously recorded, and you have over a long enough period of time that you have reproducible observations, not just off one anecdote.
[Damien Blenkinsopp]: Thank you there for some great insights into randomized controlled studies, and the averages also, which comes up sometimes on this show. Averages don’t necessarily mean you. So thank you for reinforcing that point.
Rob, thank you also for making time available today. I really enjoyed this show. You’ve obviously got a very, very deep background in this stuff, and we covered a lot of material. Looking forward to read your book also.
[Rob Knight]: Okay, great. Well thanks Damien, and thanks again for your interest in this, and this is only going to get more exciting as we find out more and more about the microbiome.