The mitochondria is often described as the “powerhouse” of the cell and it supplies the energy the body needs to function properly and efficiently.
Previously, we have discussed mitochondria as related to cancer, in episode 16 with Dr. Thomas Seyfried and in episode 3 where Dr. Terry Wahls described mitochondrial health and the link to autoimmune disorders.
This episode will focus on mitochondrial function and the symptoms we experience when our mitochondria have sustained damage from either environmental factors, natural aging, or other exposures. Often this leads to general fatigue, cognitive decline, or physical decline and the effects can be seen in patients who suffer from chronic fatigue illnesses, neurodegenerative disorders, cancer and various other diseases.
Lipid Replacement Therapy (LRT) has been shown to repair the mitochondrial membrane damage and improve symptoms for many patients suffering from these chronic diseases and other natural aging symptoms.
– Garth Nicolson PhD
Today’s guest is Dr. Garth Nicolson who is an extremely accomplished research scientist best known for his work with Gulf War Syndrome, and Lipid Replacement Therapy (LRT). He is the president, founder, chief scientific officer, and researcher at The Institute for Molecular Medicine in Huntington Beach, CA where he conducts most of his current research.
He was the leading authority serving the United States House of Representatives on the study of the cause, treatment and prevention of Gulf War Syndrome on suspicion of biological warfare. For his service he was conferred honorary Colonel of the US Army Special Forces and honorary US Navy SEAL.
He has published over 600 peer reviewed research papers and served on the editorial boards of 30 scientific journals. In 2003 he introduced LRT and its benefits for the first time, shedding light on the importance of mitochondrial function and repair of damaged membranes and its benefits for aging, cancer and chronic disease states.
The episode highlights, biomarkers, and links to the apps, devices and labs and everything else mentioned are below. Enjoy the show and let me know what you think in the comments!
What You’ll Learn
- Mitochondrial function decline is the underlying problem in many chronic diseases (6:43).
- Mitochondria are the powerhouse of the cell providing energy – like a battery – which fuels the cell’s function (7:43).
- Oxidative damage to the lipid membrane of the mitochondria is the most universal cause of damage (8:38).
- Damage to the lipid membrane harms the phospholipid molecules causing “leakiness” across the membrane (11:30).
- If you don’t produce enough energy in a cell, you lose the function of that cell (13:15).
- Damage to the energy process in a system can occur during aging, chronic illness, viral/bacterial infection, toxic exposure, etc. (13:55).
- Some patients have restored their endocrine systems by repairing their mitochondria in some way (15:53).
- Chronic fatigue illnesses (chronic fatigue syndrome, fibromyalgia, etc.) are directly related to loss of mitochondrial function, which is mostly true for many other diseases as well, such as cancer and neurodegenerative disorders (16:45).
- Much of the mitochondrial function decline occurs because of the natural aging process (18:46).
- For instance, improving the function of a 90 year old, fatigued patient greatly improves mental and physical functions for the patient (19:01).
- Repairing the mitochondrial function for patients who have any of these diseases is not a cure-all, however it is a step in the right direction and definitely supports the overall recovery for the patient (21:21).
- Dr. Nicolson discusses the importance of lipid replacement therapy (LRT) as a way to replace damaged membrane phospholipids to improve mitochondrial function (22:48).
- LRT also functions to detox and repair chemically damaged cells as the lipids delivered to the system can soak any chemicals out from the membranes and remove them from the body (27:11).
- Dr. Nicolson works with populations who have had particular exposures however everyone has been exposed to various chemicals throughout their lifetime (31:05).
- Using both LRT and infrared saunas can speed up the long, slow process of detoxification and recovery (32:47).
- LRT can reduce the symptoms of detoxification and recovery; for example LRT used in conjunction with chemotherapy for cancer patients helps the patient manage the side effects of the cancer treatments (34:50).
- Patients generally see improvement of symptoms between 10 days and 3 months after the start of LRT but when therapy is removed the mitochondrial function declines again and symptoms return (36:39).
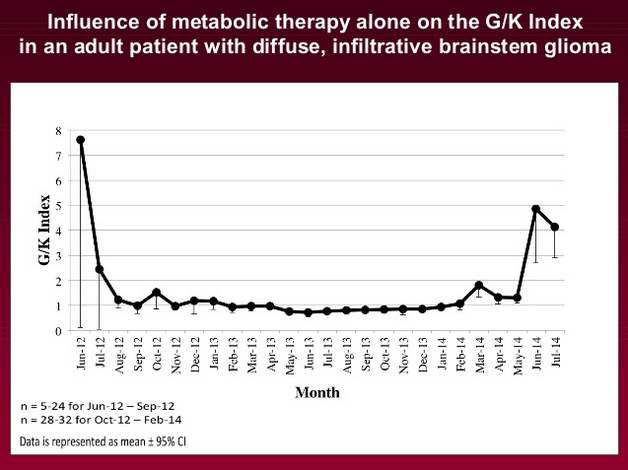
- Mitochondrial function can be measured directly by testing the mitochondrial membranes in the white blood cells (38:38).
- LRT is becoming more popular especially with naturopathic doctors and individual people as you do not need a prescription to obtain these natural supplements (40:37).
- An increased dose of lipids is crucial for patients with severe chemical damage or mitochondrial damage so luckily no one has reported negative side effects yet as lipids are natural substances of the body anyways (44:37)!
- Cholesterol markers and homocysteine levels have been shown to improve when using LRT (45:48).
- LRT is proving to be effective as an anti-aging treatment, a therapy for various diseases processes, and as a co-treatment option for cancer patients to reduce negative side effects and fatigue related to traditional therapies (46:29).
- LRT works well at improving energy systems however dosages, etc. do have to be optimized to work with each person’s unique system (50:26).
- LRT is a lifelong solution and a long term treatment because we are constantly exposed to new toxins, infections, and traumas throughout our lives (52:17).
- The minimum supplement needed for LRT is NT factor lipids. (55:32).
Garth Nicolson PhD
- Garth Nicolson PhD
- The Institute for Molecular Medicine: Founded by Dr. Nicolson in an effort to help fight chronic disease through research and discovery.
- Garth Nicolson Research: general PubMed results for Dr. Nicolson.
- Garth Nicolson LRT Research: PubMed research results in regards to LRT.
Tools & Tactics
Interventions
- Lipid Replacement Therapy (LRT): Used to restore and repair mitochondria function by replacing damaged lipids in the membrane and restoring the mitochondria’s ability to produce energy for the cell. (See relevant lipid supplements below).
- Infrared Sauna: Used to remove fat soluble toxins in particular from the body. Garth Nicolson recommends using this along side LRT to help with the removal of chemicals from the cells, which tends to improve results.
Supplements
- NT Factor EnergyLipids: NT Factor is the lipid based supplement that is the main component used in LRT. There are a variety of products including this one, which contain NT Factor. Read more about these on NTFactor.com, as recommended for use by Dr. Nicolson.
- NT Factor Energy Wafers: The specific NT Factor product that is “child friendly”, as the wafers easily dissolve in the mouth and do not need to be swallowed.
- ATP Fuel: In addition to NT Factor, this supplement also contains NADH and coenzyme Q10 which also aid in the energy production cycle in a cell.
Tracking
Biomarkers
- Cholesterol: A cholesterol panel covers a number of markers related to lipoproteins (such as HDL and LDL) in the blood. LDL and HDL are standard markers used to track cardiovascular risk. Dr. Nicolson has seen LDL drop and HDL increase with use of LRT – which typically indicates improvement and lower cardiovascular risk.
- Homocysteine: A marker often used to assess cardiovascular risk. Higher values relate to increase cardio risk. This marker is often related to methylation SNPs like MTHFR as discussed in episode 5 with Ben Lynch. Dr. Nicolson has seen homocysteine levels drop with LRT also.
- Mitochondrial Membrane Potential: An approach to assessing the health and functioning of a cell’s mitochondria by looking at it’s potential or voltage. In the same way as with a battery, if it is functioning, the outer membrane of mitochondria has an electric output and thus a voltage.
Lab Tests, Devices and Apps
- Inner Mitochondrial Membrane Potential via Rhodamine 123: The status and functioning of the mitochondria are assessed via analysis of mitochondria inside white blood cells with the dye rhodamine 123 and a fluorescence microscope (see study here). The test provides a quantitative fluorescence value indicating the health of the mitochondria and integrity of the membrane. This test is not easily accessible and is used for research purposes.
Other People, Books & Resources
Organizations
- Researched Nutritionals: This company produces some of the products that contain NT Factor, including ATP Fuel.
Full Interview Transcript
[Garth Nicolson]: Well it’s a pleasure to be on your program.
[Damien Blenkinsopp]: To start off with, I was really interested to find out how you first started working with mitochondrial function. Where it first came up for you, and you started taking an interest in it.
[Garth Nicolson]: Well this really goes back to our work on Gulf War veterans. And from that we did work on civilians with Chronic Fatigue Syndrome, Fibromyalgia Syndrome and related fatiguing illnesses. And one of the underlying problems in all of these – and it turns out any chronic disease – is mitochondrial function. There’s just not enough energy around to provide all the necessary high energy molecules in a cell to perform all the functions necessary.
Then you get into energy deficits, and if the energy deficits are systemic, well you can have a chronic condition with lack of energy, lack of mental alertness, all kinds of other additional problems. Because basically every cell requires energy to perform. And some cells, such as the nervous system, require a lot of it – six times what most cells require – and so they’re particularly sensitive to losses in energy function.
[Damien Blenkinsopp]: It sounds like there’s a wide variety of symptoms that could be reflecting some kind of mitochondrial function damage, or interruption. Is that the case? Is it quite a wide variety of symptoms?
[Garth Nicolson]: There are a wide variety of symptoms associated with loss of mitochondrial function. And as I mentioned before, the mitochondria provide energy to your cells. In fact, almost all the energy is provided by mitochondrial function in our cells.
If you’re breathing oxygen, you’re using that oxygen to provide it to mitochondria, so they can convert it to energy, along with other molecules that they use in the process called Electron Transport System. And it’s a complicated conversion system which converts, essentially, stores that you have in your cells to high energy molecules that you need for doing a number of different functions.
Now in different clinical conditions, we find that these people have given signs and symptoms, but often they’re also related to mitochondrial function, because a lot of these problems arise when there isn’t enough energy left for cells to perform their functions necessary, and consequently this can have profound effects.
[Damien Blenkinsopp]: Right, and what kinds of damage can interfere with mitochondrial function?
[Garth Nicolson]: Well there are a variety of different types of damage. We’ve concentrated on damage to the lipid membrane of the mitochondria, because this turns out to be the most sensitive form of damage, or the most universal form of damage that we find in mitochondria. They’re particularly sensitive to oxidative damage.
And oxidative damage can occur, for example, during infection, during high performance issues, if you get run down – for example, physically, mentally, you name it – or because of infections or other damages, disease associated damages, mitochondrial function suffers. And in order to recover from all of these, you do have to have mitochondrial function available, because you can’t repair and recover without it.
[Damien Blenkinsopp]: So are we all constantly repairing the lipid membranes, as you are talking about? Is this a constant? Because when you mentioned, for instance, high performance, could that be someone like an athlete, or someone who’s heavily into fitness? Are they constantly causing this type of damage with oxidative stress, which then has to be repaired?
[Garth Nicolson]: Well, that’s true, but it’s also true during aging, for example, where our membranes normally get damaged during aging processes. And mitochondrial membranes are particularly sensitive to aging, and as we age, they get more damaged. And so if you look at a 90 year old, many of these 90 plus year old people have lost almost half their mitochondrial function.
And a lot of that is due to accumulated damage in the mitochondria, and a lot of the damage is due to the damage to the mitochondrial membrane. And the inner mitochondrial membrane is integral to our production of energy, and if that’s damaged, they become leaky, and lose function, and they can’t maintain the trans-membrane potential, the electrical potential across the inner mitochondrial membrane, which is absolutely necessary to produce high energy molecules.
[Damien Blenkinsopp]: Right, right. Well to take a step back, when you’re talking about trans-membrane, what’s the function of the membrane in terms of generating electricity? Because basically the mitochondria are a bit like our power cells, you know our batteries, which feed our cells and the rest of our body with energy. But how do they do that, and what’s the role of the membrane in that process?
[Garth Nicolson]: Well I always liken mitochondria to the little batteries inside our cells. And like any battery, it has to be insulated to selectively permit a trans-membrane potential across different membranes in our mitochondria. It’s a biological membrane instead of a synthetic membrane that we have in batteries, but it provides the same kind of insulation necessary to separate electrical charges.
And so when this separation of electrical charges occurs, you can make a battery out of it. Essentially that battery drives the production of high energy molecules in the mitochondria just as it does in a normal battery.
[Damien Blenkinsopp]: Great. And what types of damage are we talking about when we’re talking about this membrane getting damaged?
[Garth Nicolson]: Well there’s certain molecules in the membrane. It can be the phospholipids that make up the matrix of the membrane. But when they’re damaged, there can be enhanced leakiness across the membrane. So it’s like you get a leakiness if you take the insulation off a battery it will leak, and you’ll lose the charge of the battery.
The same thing in the mitochondria. If they become leaky, and the inner membrane becomes leaky, you can lose the trans-membrane potential, and then you can’t form the high energy molecules. There are also some critical lipid molecules, like cardiolipin, that are exquisitely sensitive, in fact, to oxidative damage. And when they’re damaged, this results in loss of function. So these different types of things are very important, the direct function and the trans-membrane potential.
[Damien Blenkinsopp]: So these are different types of fat molecules that we need in the membrane for it to function optimally. And it’s kind of like holes have been punched in the surface of the membrane, and molecules have been knocked out of it? Is that a way to look at it?
[Garth Nicolson]: It’s a little more subtle than that. When oxidative damage occurs, think of the lipid chains that are going into the membrane, into the hydrophobic matrix of the membrane, you can think of kinks getting in those chains after they’ve been oxidatively damaged. And those kinks mean that the lipids can’t fit together as well, and there’s a certain rate of leakiness across the membrane.
[Damien Blenkinsopp]: Great. Is this something anyone should be concerned about, in terms of the type of damage? You just referred to a 90 year old, the damage that’s gone on to them.
What kind if symptoms could someone think of if, maybe they don’t have a chronic disease like some of the ones you referred to, but are there other indicators that potentially they have some aspect of mitochondrial damage, in terms of some symptoms they could look out for which might identify that?
You were referring to, like brain fog, or other symptoms. Are there obvious ones, or is it always very different, and it’s kind of difficult to differentiate this to other things that might be going on?
[Garth Nicolson]: Well, obviously a number of different factors can cause problems with your central nervous system, for example, your peripheral nerves and other systems of your cells, but one of the things that can happen is that if the energy systems inside the cells get run down, they don’t function as well. It’s as simple as that.
So if you don’t produce enough energy in your cells, your cells can’t function as well. So all the different functions that cells do, of course the nervous system, the function is to transmit nerve impulses, if they’re not functioning properly then the nerve impulses can’t be transmitted properly. And so that leads to a loss of function.
Now this can occur when people get run down. And they can get run down for a variety of reasons. They can lose their energy stores, for example, or they can have them damaged through the mitochondrial damage that I was talking about. Some of this occurs naturally, and it’s reversed by rebuilding things like the membrane as it’s damaged.
And if there’s some process that prevents that rebuilding of the membrane, then this will persist. For example, during infection we know that a variety of different types of infections – viral, bacterial and so on – cause an increase in the what are called reactive oxygen species, or ROS. And these damage the membranes of the cell, and in particular they can damage the inner mitochondrial membrane and cause loss of function.
So these are things that can happen. So it can happen during infection, it can happen during aging, it can happen during a chronic illness. It can happen when you get run down, for example, or you have exposures of various types that are toxic. So under a variety of different conditions you can have damage done to your mitochondria, which means loss of function, and your body cannot repair itself as well without that energy that’s necessary to do it.
[Damien Blenkinsopp]: Great. And I guess an important differentiation I just wanted to point out here is a lot of people talk about adrenal fatigue, and if one of the symptoms is fatigue, basically having low energy – which I guess would be one of the outputs of mitochondrial damage – how do you differentiate it, or is it possible to differentiate it, to something which someone would diagnose as adrenal fatigue? Or how do you look at that?
[Garth Nicolson]: Well they go hand in hand, because for the adrenal gland to function, it requires energy. So if there’s an energy deficit in the adrenal gland, then that’s not producing the correct hormones and everything that your body needs. Cytokines and so on. So this sends up the deficit, and this can cause a problem. So they’re inter-related.
[Damien Blenkinsopp]: Right, right. And it sounds like you’d think mitochondrial damage might be a pre-cursor to adrenal fatigue, often.
[Garth Nicolson]: It could be a pre-cursor to adrenal fatigue. And so we’ve seen people that have managed to repair their endocrine systems by repairing their mitochondria. So at least we know, and at least in some patients, that’s reversible.
Now in other patients they may have either genetic defects, or toxic exposures, or something like that, that’s damaging specifically those particular adrenal glands. So that’s a different issue. But we do know that these things are inter-related. If you don’t have the energy, you can’t repair.
[Damien Blenkinsopp]: So you’ve worked, in your clinical studies and your patient population, you’ve worked with Gulf War illness and Chronic Fatigue Syndrome and some others. Could you give us a brief explanation, for the audience, what are the issues that these people have? How critical are they, what kind of situation are they in? Before we talk about the lipid replacement therapy and what it was able to do.
[Garth Nicolson]: Well there’s quite a bit of variation on the signs and symptoms of people with chronic illnesses, and a variety of different sorts. We started working with what are called Fatiguing illnesses, because Chronic Fatigue is the hallmark of those illnesses, and that’s directly related to mitochondrial function. So that was a good place to start.
A lot of other diseases, mitochondrial function may be thought of as a side issue; although it’s important it may not be the primary clinical manifestation of the disease process. Nonetheless, it’s still important [for] practically any chronic illness.
If you take something like a neurodegenerative disease, for example, mitochondrial function is intimately tied up with neurodegeneration. You cannot repair your nervous system if you don’t have the energy available to do it. So if mitochondrial function goes down, you’re particularly susceptible to neural damage. And to have that process going on, it can exacerbate it.
So this is one of the things that we are trying to work with, how to improve mitochondrial function, how to help people with a variety of chronic illnesses.
So we started with the fatiguing illnesses, and Gulf War Illnesses are really one of the fatiguing illnesses, but Chronic Fatigue Syndrome is another one, Fibromyalgia syndrome is another. Fibromyalgia syndrome is a little different because it’s also characterized by widespread pain, in part, we think, that’s due to mitochondrial function problems as well. The nervous system not operating properly. But there are some other factors as well.
So all these issues have as an underlying commonality loss of mitochondrial function. In a variety of different diseases, that’s true. And it’s true in infections, it’s true in toxic exposures, it’s true in a wide variety of different diseases. Cancer, you name it, practically every disease you can think of has a problem with mitochondrial function. They can’t keep up the repair process.
[Damien Blenkinsopp]: Are there other, beyond the ones we’ve already discussed, are there other types of patient populations, or other use cases you’ve looked at for lipid replacement therapy? You mentioned anti-aging as well. Have you worked with people for that area also?
[Garth Nicolson]: Exactly. Well, anti-aging is probably the normal manifestation of mitochondrial functions. I mentioned as you age you lose mitochondrial function naturally. And there’s an increase in the oxidative damage that occurs in all of our cells, so we need to reverse that process.
And so, one of the things we’ve done with the aging process is we’ve taken people that were fatigued, 90 years old plus, we’ve improved their mitochondrial function to a 30 year old. And they’ve gained all kinds of function in the process. Mental function, physical function, you name it. Every system that seems to be important improves.
[Damien Blenkinsopp]: In terms of the studies you’ve done, are these all based on studies, or is some of this based on patient population, other studies? Because I’ve seen some of your presentations, looking at your studies and work on the fatigue cases and the Gulf War Syndrome. So are all of the studies basically based on those patient populations versus the anti-aging, or have you also done studies on anti-aging also?
[Garth Nicolson]: Well we’ve done some studies where we’ve included older people in our studies, and that’s where we see the anti-aging effect. So with those older cohorts of patients – well they really are, they’re subjects, not patients, because their main problem is they’re elderly and they have fatigue issues. So we can’t categorize them as a disease process, because it’s a natural process of aging.
So they are fatigue subjects. So they have chronic fatigue, but they don’t have a disease called Chronic Fatigue syndrome, or Myalgic Encephalopathy, or something like that. They have fatigue problems. So we work with people like that as well.
We’ve also worked with cancer patients, we’ve worked with people with chemical exposures, we’ve worked with people with infections. For example, there are a wide variety of chronic infections that we work with, like Lyme disease, mycoplasma infection, so on and so forth. Were, again, in the chronic disease process, it’s always an issue. Mitochondrial function is always an issue.
[Damien Blenkinsopp]: Right. Would you say it’s going to be helpful in most situations to have some kind of lipid replacement therapy as a support for your mitochondria? In terms of the disease process, to give an idea, what kind of results do you get from people? Can you get people back to resolution? Or is this basically managing symptoms, managing the damage of mitochondria, kind of therapy?
[Garth Nicolson]: Well it depends on the situation. If we take normal, healthy people that can get run down for one reason or another, yes we can bring them completely back by repairing their mitochondrial function.
If you take people that are in a disease process, usually these processes are much more complex than just mitochondrial function. Mitochondria being one part of the problem that they have. And we can repair that part, but there are other elements that have to be taken care of as well. For example, if you take somebody with a neurodegenerative disease, does just repairing their mitochondria reverse the process? No. There’s some other elements that are involved.
Does it help? Yes, it seems to help people with cognitive loss and so on and so forth. But it doesn’t reverse it or completely cure the problem. That would be a pretty simplistic approach to these complex, multi-factorial issues. But, we do know that this is an important element in all of these processes.
[Damien Blenkinsopp]: Do you feel like it provides a support to get people to recovery? That it’s an important ingredient in your practice? You feel like it helps people to recover by giving them that mitochondria energy, thus supporting things like the immune system, and other systems of the body?
[Garth Nicolson]: Absolutely. If you’re talking about the immune system, for example, it requires energy to function. So if your energy goes down, your system might be less capable. So, it’s absolutely important there.
And it’s absolutely important for any type of recovery, because what is recovery? Generally it’s repairing our cellular processes and our system processes, our organ processes, and that requires energy. That just doesn’t happen naturally without energy.
[Damien Blenkinsopp]: Okay, so let’s get kind of concrete here, for the audience listening at home. What is lipid replacement therapy? What does that actually involve, what do people do when they’re taking lipid replacement therapy?
[Garth Nicolson]: Well this is a particular type of lipid, this is not just the normal gross lipids that people might think of. These are very particular membrane lipids, so these are lipids that make up the membranes of all our cells. And of course as I mentioned before the membrane is an integral part of the mitochondria, but they’re also an integral part of other organelles within the cell.
Membranes, in fact, are absolutely essential for the function of all of our cells. And they get damaged, they get run down, we have to replace the molecules and the membrane occasionally. And some of the most sensitive molecules are the lipid molecules, because they’re very sensitive to oxidative damage, which can occur in any disease process, infection, or whatever.
So this is something that has to be replaced. And we came up with this idea, well we need to replace the membrane lipids, which are primarily a class of lipids called glycerophospholipids, that don’t need a lot of other things. That’s what we need to help repair the, more or less the matrix of the membrane.
So if we supply that in purified form, undamaged form – which is very important – then we should be able to help repair this process, because we have natural systems in our body to replace these lipids as they’re damaged. Because we evolved with the mechanism to help repair and replenish our membranes.
The problem is we can’t keep with the damage, and that’s when the disease process can occur. So to help it along, if we provide the lipids, well we can help that process.
Now people say well, you can buy all kinds of different stuff at the store. Well, the reason it doesn’t do it is a lot of those lipids are already damaged, they’re already oxidized, they’re not the right kind of lipids, and so on. So they’re not very helpful. And even a lot of supplements that people buy in the store are not very helpful, because even if they have lipids they’re not the right kind of lipids, or they’re already damaged, or they’re damaged during the shelf-life.
These are very sensitive issues, which we’ve tried to overcome with the products that are designed to survive and provide our bodies with exactly the right lipids that we need to repair our membranes and restore function.
[Damien Blenkinsopp]: So, would it be correct to, because you provide these in pill form. So is it these are things we can get from food, but we get them in very low quantities, so it’s like having a very high dose of the reduced form? The active form versus the oxidized form of these lipids?
[Garth Nicolson]: Well that’s part of it, but a lot of the lipids are damaged already by the time we take then in in the foods, and unfortunately, our transport systems, they can’t readily acknowledge a damaged lipid from a properly pristine, undamaged lipid. And so a lot of these things might get transported in as well. Or at least they’re transported in, too much of it is transported in if it’s damaged.
So we kind of flood the system with undamaged lipids, and that helps the whole process move very smoothly. It also helps remove the damaged lipids, which is one thing we’re working on now, is how to take people who are chemically damaged – and I can talk about that later – help them remove those damaged chemicals from their bodies.
And it turns out that the replacement therapy can help do that, because it’s an energy driven process, so it helps provide energy, but it also is very dependent upon moving what we call hydrophobic molecules out of the cells. And the lipids that we provide have a very important part of their structure, a hydrophobic part of their structure, which helps remove these molecules.
So if they’re present in quite a bit of excess it can help remove these damaging chemicals from our system. And that’s one thing we’re working on right now.
[Damien Blenkinsopp]: That sounds very interesting. We’ve spoken about detoxification before. So, just to take a step back, when you say chemically damaged people, what kind of things has happened to these people?
[Garth Nicolson]: Well often people with chemical damage due to illness could be anything from herbicides, for example, to very industrial chemicals, and so on and so forth. Often damaging chemicals are chemicals that we would classify as hydrophobic chemicals. That is, they don’t like water. They like fat, essentially.
So they concentrate in our membranes, they concentrate in the fatty parts of our cells and lipid droplets, and so on. And they can remain there indefinitely. And they can bleed out very slowly and cause problems with the cellular mechanisms. So to get rid of these, we need a system to remove them.
But the system that we have for detoxification is an energy dependent system, at least one of the most important ones. So by providing mitochondrial energy, that helps in that process. But it also helps remove them because, it turns out, the lipids that we provide kind of soak up these molecules, because it will bind to the lipids and it helps them be excreted from our cells and from our system, so they naturally come out in the GI system.
[Damien Blenkinsopp]: So that sounds like the new molecules that you’re providing are basically replacing the ones which have absorbed the toxins, the chemicals, the fat soluble chemicals, and are thereby displacing them and allowing the body to remove them.
[Garth Nicolson]: Well that’s basically it, but it’s providing a different store, or different storehouse for these chemicals to move into, but a storehouse that we can eliminate. And that’s the important thing is to do that.
One of the mechanisms for moving chemicals that’s most important for these very damaging chemicals that concentrate in our cells is that there are enzymatic mechanisms, to conjugate the offending chemicals with other hydrophobic molecules within the cells, to make them more easily removable.
Well when that happens, if we have somebody’s undergoing lipid replacement therapy, there are a lot of these lipid droplets around and lipid carriers around, which could help soak these conjugated chemicals up and remove them from our systems.
So it’s a process, it’s a very slow and steady process of removal. It doesn’t, of course, happen over night, but it’s a natural system for removal of damaging offending chemicals from our bodies. And this just takes it to a maximum advantage by providing some of the things necessary for it to operate in the first place.
[Damien Blenkinsopp]: So out of interest, because we’ve spoken quite a bit about detoxification, and also the kinds of tests involved in measuring things like mercury, lead, and other toxins. Are you able to test these chemicals in fats and see the change, and how long does it take? Does it take a month, two months?
[Garth Nicolson]: Again, we’re not talking about heavy metals, because that’s a different process of removal. We’re talking about chemicals that partition themselves into the fatty portions of your cells. Well these chemicals, and they could be, for example, herbicides or any number of different chemicals.
[Garth Nicolson]: Yeah, a lot of the chemicals that damage our cells are very hydrophobic, and they partition into the fats of the cell, the fat systems and the membranes of the cell. They have to be removed or eventually they’ll interfere with the function. That removal process is slow. It does not happen over night.
So it’s a very slow process of bleeding them out and removing them from the stores, and so on and so forth. So one of the first things that you can see, for example, if you give somebody lipid replacement therapy, is you might actually see an increase in the number of these chemicals that are being excreted, that are being at least mobilized as well.
So there may be an increase in the blood levels of these, because they’re being brought out of the cells and being transported to the brush border cells in the intestines, and then secreted there. But again, there are a number of different mechanisms, this being just one of them.
[Damien Blenkinsopp]: I’m guessing this is a new area, it sounds like you’re more focused on this recently?
[Garth Nicolson]: This is a very new area of ours that we planned to get very focused on because it’s so important, so necessary to help these people, many of whom have been damaged for decades without much help at all.
[Damien Blenkinsopp]: So just out of interest, are there any specific exposures? And is it people working in factories, or is it people who have detoxification systems which aren’t functioning, or perhaps they have some methylation or other issues, which they’ve lived a pretty normal life, compared to most people. It’s not like they’ve been in any specific situation which could have exposed them to more chemicals.
What kind of populations are you dealing with here?
[Garth Nicolson]: We work with the populations that are sick in general, although a variety of different individuals may be exposed to chemicals, because they are all over the place in our modern environment. And people will have tremendous variation in their sensitivities to these chemicals.
So you may have somebody that’s been normally and naturally exposed who’s becoming sick because of it, and other people not at all. Because there’s such a range of sensitivities to these.
So we’ve worked with people who’ve had specific exposure. For example Vietnam war veterans who’ve had exposure to Agent Orange, which is a particularly nasty chemical that takes a long time to remove from the body. Or Gulf War veterans that are exposed to petrochemicals in the forms of fumes, and exhausts, and oil fires, and so on and so forth, during the first Gulf War, and some during the second Gulf War.
So these are people that have had chemical exposures above and beyond the normal types of exposures that we might see. But in the industrial environment that we’re in, there are a lot of people that get exposed to various chemicals.
If you work in the petrol-chemical industry, for example, you could be exposed fairly easily, and it may not cause any problems with you but there are other individuals who have severe problems because of it.
So again, there’s a wide range of different sensitivities to these different chemicals that are seemingly in our population.
[Damien Blenkinsopp]: Great. I just want to bring it up, because I know a lot of people talk about infrared saunas, and saunas in general when it comes to fat detoxing from the fat soluble toxins like the ones we’re talking about. So, do you have a viewpoint on that, on the effectiveness of infrared sauna? Is it something you’ve ever gotten involved with, and could you compare it to your process?
[Garth Nicolson]: We’ve looked a bit into that, and yes the use of infrared saunas to actually bring the chemicals out in your sweat, which is what it really does. But if you do these at least a minimum two times a week, you’ll slowly start to deplete some of the chemicals from your body.
What we found is if you add our lipid replacement therapy on top of that, you can accelerate the process of removing the chemicals from your body that way. So again, this can be an adjunct to a variety of very well established methods for detoxification.
[Damien Blenkinsopp]: Great. Have you seen complete recoveries, or to what degree have people recovered from their health? Because we’re talking about people that are quite sick.
[Garth Nicolson]: Well, we’re in the beginning process of this right now. So this long term goal of ours, but again, this is just the beginning, and we’re seeing some responses. We’re seeing people that are feeling better, getting better. But again, it’s a long, slow process for recovery.
And again, there may be other types of damage along the way that we discover that these individuals have. Most of these chronic illnesses are multi-factorial. There’s not just one problem, generally these people have a number of problems, this being one of them. But this is something that we can approach.
[Damien Blenkinsopp]: Absolutely. So it sounds like an on-going process of a year. We’re talking really long term, just to give people an idea.
[Garth Nicolson]: We’re talking long term. Particularly when it comes to removing offending chemicals from your body, it’s a long term process. Same thing with removal of heavy metals from your body, it’s not a short term process.
It can take years to remove heavy metals from your body, and the same thing is true with chemicals that build up in your body. It can take a long time to really get rid of them. And in fact, if you mobilize them too quickly, you can really make people feel sick in the process. So it’s better to do it naturally and slowly.
[Damien Blenkinsopp]: So, I’m glad you brought this up, because we’ve spoken about these kind of topics quite often on the podcast before. It’s nice to get that. Is there anything you have to do in terms of supporting them?
Because you mentioned that some people can get sick if it comes up too fast. Is there anything else that you do for them while you’re using the lipid replacement therapy to support detox, or as long as you go at a reasonable rate, which I imagine is a reasonable dose?
[Garth Nicolson]: What we have found is that lipid replacement therapy actually reduces the symptoms of detoxification, reduces the symptoms, for example, of cancer chemotherapy. So it is very significant in our studies with the cancer patients. They’ve showed really quite a dramatic decrease in the side effects due to chemotherapy, because it causes a lot of damage to our normal systems, and the lipid replacement therapy helps repair those normal systems.
So you get a reduction in the associate problems, very adverse events that occur during cancer therapies. So, you could figure that is, again, when you’re repairing the normal mechanisms of the cells, the tissues, and this helps the overall process.
[Damien Blenkinsopp]: Right, right. So you’re saying a lot of the symptoms people have when they’re going to a detoxification process, or, as you’re saying, chemotherapy or exposure to other toxins or when they’re ill, is due to mitochondrial damage, right?
So when you’re supporting the mitochondria with lipid replacement therapy, it helps to manage the symptoms as well in that process and reduce them, because there’s not as much damage going on.
[Garth Nicolson]: Well it does, and not only that, it helps accessory systems as well, because a lot of the signs and symptoms that we see that are associated with damage are release of chemical messengers like cytokines, that cause all kinds of problems in the body, and so on.
And damaged tissues can initiate this whole process. So if you reduce the damage, you can reduce these accessory damage response systems from exacerbating the signs and symptoms in these patients.
[Damien Blenkinsopp]: Great. One thing I wanted to kind of make clear to people, what kind of results, because when I was watching some of your clinical studies you were looking at. Over the few months you were giving lipid replacement therapy, could you talk about what kind of impacts it generally has on the people?
If we’re talking about say the chronic fatigue, or in the Gulf Syndrome cases, the ones I saw, what kind of time-lines did you walk through in your clinical studies? And also, it was interesting what happens when you stopped the therapy.
[Garth Nicolson]: This is a process that takes time. You don’t repair your mitochondria overnight. It takes days to weeks. The process can begin fairly soon after you take the lipid replacement, but it takes time to fully repair the mitochondria.
And we’ve seen, again, that it can take, depending upon the different formulations of lipids, anywhere from 10 days to three months, depending on the formulation, depending on the patient type, to reach an equilibrium of repair. And these people see a maximum benefit in that time. But they do see benefit fairly, fairly soon.
[Damien Blenkinsopp]: And then what happens when you stop the therapy? Depending on the condition. So when it’s in a chronic condition, like Chronic Fatigue Syndrome, or Gulf Syndrome, where they have some kind of infection or some underlying cause, then what happens when you stop the therapy?
[Garth Nicolson]: Well then it slowly returns back. As the mitochondria get damaged again, it will slowly go back to the way it was before you started the therapy. And one of the trials that we did was called a cross-over trial, where we take patients, and they’re on part placebo and part the lipid replacement therapy, but they don’t know when they get it.
And what we found was when they get the lipid replacement therapy, they improved. They had reductions in fatigue with 35 to 45%, enhancement of mitochondrial function was a little bit less than that in terms of percentage, but very significant. But when we switched them to placebo, it slowly started to go back again.
[Damien Blenkinsopp]: Yeah.
[Garth Nicolson]: And they wondered what was going on, because it wasn’t having the same effect. So we could prove that it was in fact the lipid replacement therapy that was giving them the benefit, not a placebo effect.
[Damien Blenkinsopp]: Great, thank you very much for that. And so, what were you using to assess mitochondrial function in terms of tests?
[Garth Nicolson]: Well what we do is we take a blood sample from patients, we isolate the white blood cells which have mitochondria – the red blood cells do not have mitochondria – and we can measure the mitochondrial function directly.
And what we’ve done actually, more recently, is we’ve measured the membrane potential of the inner mitochondrial membrane using a special redox dye, called rhodamine 123, and see that fluorescent dye in the mitochondria. If the mitochondria are fully functioning, they will reduce that dye and it will fluoresce.
And if they’re not functioning, they can’t reduce it, and the mitochondria won’t fluoresce. So you can see it visually in a microscope and you can quantitate the fluorescence so we can get a quantitative value.
[Damien Blenkinsopp]: Great, great. So this is your own lab tests that you developed for this purpose?
[Garth Nicolson]: Well other people really developed the tests, we just adapted it to what we were doing.
[Damien Blenkinsopp]: Great. Well I guess what I wanted to say is it’s a pretty unique [test], like we wouldn’t expect to find it outside of research, apart from potentially your practice, and some other specific areas.
[Garth Nicolson]: This is a very specific research type of test, and you won’t find it in your normal doctors office, that’s for sure. Because it requires some complicated machinery, like a cell sorter and fluorescent tools, fluorescent light sources, and so on and so forth. So, it’s a bit complicated, but it works in a research environment.
[Damien Blenkinsopp]: So it’s not something you use on your patient population, I guess it’s cost prohibitive. It sounds like quite complex.
[Garth Nicolson]: Well it is, and speed is very important. So you have to have a very fresh sample. Often if you’re not doing the test immediately or soon, you could get variable results. So to get the best results, speed is very important. So, generally you have to have this complicated equipment on hand to do it. And the technical expertise to do it.
[Damien Blenkinsopp]: So, how well accepted is lipid replacement therapy? We’ve spoken with functional medicine doctors here, and we’ve looked at functional medicine quite a bit, contemporary medicine is there of course also, and in the research studies.
Is there a lot of support for it right now, or is it still something quite niche that basically there’s not very many people using?
[Garth Nicolson]: Well more and more are using it, because more and more people are finding out about it. And we published some 28 papers on this process. So, it’s well-known in the literature. We published a number of reviews on it now.
Less known in the general population of physicians, more in the naturopathic medicine areas, mainly because I get around and talk to these people, and then they get informed that way, through conferences and so on. So it’s becoming more and more well-known, and even people outside the medical area will find out about it through broadcasts like yours, for example.
They can buy this stuff over the counter, it’s not something they need their physician’s prescription for. These are natural supplements. It’s the lipids that are in our membranes all along. So, it’s not a drug, it’s not anything but what’s there. We just have to provide it in a way that’s not damaged.
[Damien Blenkinsopp]: Well so I’ve got to ask you the question, are you using lipid replacement therapy yourself?
[Garth Nicolson]: Absolutely.
[Damien Blenkinsopp]: Okay. How long have you been using it?
[Garth Nicolson]: Well, I’ve been using it for years now. It was very effective for me in terms of reduction of fatigue. And for example, recently I got an influenza virus, unfortunately. It kind of knocked me down, and this helped the repair process. I recovered much more quickly than normal, and so I think it’s very useful for that.
[Damien Blenkinsopp]: What kind of dose are you taking? Let’s talk about practicals here. Because I’m taking ATP Fuel, for example, because I’ve had my own issues and it was recommended to me. And your research was recommended to me, so that’s kind of where I came into it.
So I’ve been taking that for a while, the ATP Fuel. And you have the NT Factor, which is a part of that. Is that actually your company who supplies that, or is that another company?
[Garth Nicolson]: I’m in a non-profit organization. We’re not really a company, but we do consult with companies like Researched Nutritionals that makes the ATP Fuel, [and] Nutritional Therapeutics in New York which makes the NT Factor, the lipids.
In fact, the Researched Nutritionals uses the NT factor product in their own product. They add some other things as well. So, ATP Fuel is an excellent product for these chemical exposure patients. In fact, I’ve just been going back and forth with the President of Research Nutritionals because we need to increase the amount of NT Factor, which is the lipids, to that product to really help these individuals.
So what we found is that more of the NT Factor is actually better. You might want to supplement your ATP Fuel with some NT Factor Lipid Wafers. By the way this is an excellent product.
We use these with children, for example, that have autism spectrum disorders, and these children have mitochondrial function problems. They readily take these wafers, and they don’t take pills. You can’t get them to take a pill.
[Damien Blenkinsopp]: Right, right.
[Garth Nicolson]: But these wafers are very tasty, and they’re creamy, they melt in your mouth because they’re lipids. So they like these creamy things, and so we have no problem with the compliance, even with difficult cases like these autistic children.
These are things that we work with on a daily basis, and we’re trying to improve our products as we go. Recently we found that although ATP Fuel is a really good product, I’m saying for the chemically exposed individuals that we need to increase the amount of NT Factor with the lipids in that product.
[Damien Blenkinsopp]: So just for the audience, the ATP Fuel has co-enzyme 10 and NADH added to it. Obviously, say that the dose of the lipids, which you say is the most important, this is kind of the innovation here, the lipid replacement therapy.
[Garth Nicolson]: That seems to be the most important thing because if you leave that out, it’s not very effective. If you put it in, it’s very effective. So it is a combination, but it’s a critical part of that combination.
[Damien Blenkinsopp]: Let’s just talk downsides here. Are there any downsides you know to this, and are there any safety issues? I just want to make that clear in terms of, maybe if you overdose it. You’re talking about increasing a dose for chemically exposed people. Is there any downside or risk to taking a lot of this?
[Garth Nicolson]: We’ve never seen any safety issues with the NT Factor lipids. As a matter of fact, we’ve given approximately 40,000,000 doses of this to patients without any recorded evidence of a real side effect.
And the reason for that is these are natural molecules that are in our cells and our systems all along. So we’re not giving our systems anything that’s different. We’re not giving them a drug, we’re not giving them something that they don’t see all the time anyway. I don’t know that it has any toxicity.
There are some studies that had been done in animals, where they’ve been given tremendous doses, without any effect at all. And we’ve had patients that have been on, oh, up to several grams per day of the NT Factor lipids without any [negative], as a matter of fact more positive effects. Their blood lipids had more normalized, they’ve had a lot of really positive things happen to them.
[Damien Blenkinsopp]: So that’s interesting. What kind of quantitative changes have you seen in terms of, are you talking about cholesterol markers?
[Garth Nicolson]: Yes.
[Damien Blenkinsopp]: Have those changed as well?
[Garth Nicolson]: Cholesterol markers and bad and good lipids. For example, lipoproteins, we’ve seen a move in the right direction. We’ve seen reductions in a product that’s associated with Heart Disease, homocysteine.
We’ve seen in elderly patients a reduction over time in homocysteine levels, which are directly related to coronary, artery disease and heart attack. So these are some of the beneficial things that we’ve seen in patients taking this long term.
[Damien Blenkinsopp]: Great, great, thank you for that. So, are there things that you’re looking for in the next five or ten years, where you think there’s going to be some more changes or innovation? Or is there anything you’re kind of excited about the opportunity of this, to help more people or to improve it?
[Garth Nicolson]: Well we’re doing an anti-aging study right now, which I’m very excited about. It’s actually going on in Uruguay. A colleague of mine who is there is a specialist on sperm function, and he takes care of men with fertility problems. But as we age, our sperm function declines, and that’s what I’m interested in as a test model for anti-aging.
So far what we’ve seen is that even in vitro, if you take sperm they have a certain lifetime. So if you take older men they have less of a lifetime, that is they can be for a while, but then they start losing motility more rapidly than younger men. But if we put in the NT Factor in it, we can help restore the function of the sperm even from older men.
So the next step is that we’re going to go from these in vitro experiments, which are very interesting, sperm motility, to in vivo experiments where we look at actual men with fertility problems that have functional problems with their sperm motility, and see if we can help repair that process.
But in terms of it’s anti-aging, which is what I’m really looking for, long range, this is an interesting model to look at. So whenever we have systems that undergo slow degeneration, like sperm function over time, if we can reverse that process, that means that we’re having an anti-aging effect, and it’s very clear, it’s very specific, and very quantitative effect. And so that’s one of the systems that we’re looking at, and I’m very excited about.
And we also have a number of different diseases processes that we’re very interested in, and we’re trying to intervene and see if we can help. Neurodegenerative diseases is one thing I’m very interested in. That’s obviously a very long term and slow process to eventually recruit patients in that area.
Another thing is reducing the adverse effects of cancer in cancer therapy. So there are two aspects of this. If some person has cancer, often they have what’s known as cancer associated fatigue, in the absence of any therapy. And of course the NT Factor will help patients with that.
We’ve seen a 30% reduction in that fatigue with patients with long-term cancer, that have had cancer associated fatigue. But it’s really reducing the side effects of cancer therapy that is most interesting, because we’ve seen reductions in side effects to chemotherapy that are really dramatic. So there’s reductions, for example, not only in fatigue but in vomiting, and malaise, and a number of other side effects – headaches, for example, and so on – associated with chemotherapy.
I think the reason for that is we’re helping repair the normal systems very rapidly in these patients after their burst of chemotherapy. So you might ask, well does this interfere with the therapy? And the answer is no, because it turns out there’s a window of therapy which is very short for the cancer, but it’s very long for the normal systems.
So these chemotherapeutic drugs attack the cancer very quickly, but then they have lingering effects on our normal systems for months, literally, after the therapy is over. So, what this does is the NT Factor helps reverse that process of damage after the therapy.
[Damien Blenkinsopp]: It sounds like you’re saying that there’s no risk of them providing a protective effect to the cancer cells themselves, provided that you introduce a timing?
[Garth Nicolson]: Well what we do is we put it in after the therapy. Because we know the damage to the cancer cells occurs very quickly. Generally, within hours after the therapy is administered. Whereas the damage to the normal systems occurs for weeks, or even months later. So we allow the therapy to occur and then next day, the following day, we start the lipid replacement to help repair the normal systems.
[Damien Blenkinsopp]: This is really interesting work. You must be really excited about all of these projects you’ve been working on.
[Garth Nicolson]: There’s something new every day!
[Damien Blenkinsopp]: And luckily you have lipid replacement therapy to keep your energy up, so you can keep focused on them all.
[Garth Nicolson]: Well I’m taking it, and so far it’s been a real help. I know that personally. But every individual will have to see what’s optimal for them. Some people will find they have to take a bit more of the lipid replacement than other people, and that may have to do with their transport systems that bring these lipids into their bodies and cells, and everybody’s different in that regard as well.
So, the same thing with detoxification. We have systems in place to help detoxify us, but it’s working so poorly for most people, or their systems are swamped out with these dangerous chemicals and they can’t keep up with the damage, and so this helps accelerate the removal of chemicals.
And also, we know that’s an energy dependent process. So it helps rebuild the energy systems that are necessary for detoxification. Because detoxification just doesn’t occur naturally, it requires energy.
So if you don’t have the cellular energy necessary, you can give them all kinds of different things, and you’re not going to see much improvement, or at least you could see much better improvement if you repair their energy systems at the same time. So I think for any detoxification, mitochondrial repair is really important, because it really helps accelerate the detoxification process.
[Damien Blenkinsopp]: Great, great, thank you. There is a cost side of this kind of therapy.
So, in terms of monitoring, how do you assess whether someone should remain on the treatment? Is it purely based on symptoms resolution, or whatever they’re trying to achieve, or do you have any markers? You brought up the homocysteine, for example. So if they had raised homocysteine and it leveled out, you could say, okay now I can take you off the therapy, because you’ve got to that critical [point].
[Garth Nicolson]: Well, actually, here’s the problem that we have in the modern environment. We don’t stop people from being exposed. We don’t stop people from getting sick, we don’t stop people from getting into automobile accidents, or whatever. We can’t do that, but what we can help them do is repair once it occurs.
We can help repair and accelerate the healing process due to trauma. We can help the healing process due to infection. We can help the process due to long term treatment of a chronic condition. All of that means that this is a long term solution, not a quick fix. And that’s why I’m taking this for the rest of my life.
And I put my father on it when he was 92, and he had much better cognition, he had less fatigue issues, and was more ambulatory, and clearer thinking, and so on and so forth. And he lived another eight or nine years. He was a coronary patient and he was on his last legs when he started.
So I think it’s never too soon. Just like it’s never too soon to stop smoking, it’s never too soon to start taking lipid replacement therapy. And yes, you may have to take it for the rest of your life if you want the benefit.
[Damien Blenkinsopp]: Well, I think I’m certainly going to stay on it. And I’m very glad to have you on the show to spread the information about this. It’s been very useful to me.
In terms of other people who, besides yourself, you would recommend to talk to about mitochondria, or lipid replacement therapy. Is there anyone else who’s done work which you would reference which is interesting, that have done a lot of work in this area?
[Garth Nicolson]: People can go to our publications, because they can see what we’ve cited in terms of the references, and the groups, and so on. Yes, there are other people working on different aspects of it. For example, there are some groups in Europe that are using intravenous lipids – similar type but not the same – and they’re getting very good results with that.
We prefer the oral supplements because obviously you can’t go in every day for an intravenous lipid replacement therapy. So, we prefer people take it orally, because we know we have the mechanism in our brush border cells lining our guts to bring these lipids in naturally, because they’re essential lipids. So, this is a very natural process that we’re supplementing, essentially.
And I think people need to find out about this. The ATP Fuel that you mentioned is primarily available through physicians and naturopaths, and professional health people, but there are also a lot of people out there maybe listening that want to know where can I get this stuff on my own.
And there’s a website called NTFactor.com, where they can buy all these products over the counter, because they’re just natural supplements. And so, that’s where they can go, NTfactor.com to find these lipids replacement therapy products, and find out more about it. And they can go to our website, the Institute for Molecular Medicine, which is www.immed.org. It’s like a media .org, and they can see the scientific results and the clinical trials.
[Damien Blenkinsopp]: Great, thank you so much. We’re going to put all of this in the show notes so people have all the references to everything we’ve spoken about today. Would you recommend they take the straight version of NT Factor? Because there’s these different combinations of things.
[Garth Nicolson]: Well it depends on what people want to do, and it also depends in a lot of cases on what people could afford if they’re buying supplements and stuff. The minimum thing they need is the NT Factor lipids.
Now, the more complex formulations like the one you’re taking cost more because they have a lot of other ingredients that are very costly. But if they want the initial punch, they need to take at a minimum the NT Factor lipids.
[Damien Blenkinsopp]: I see, that sounds like the big lever.
So Garth, thank you so much for your time today. Just on a personal note, are there any data metrics that you track for yourself? Either on a routine basis or a once yearly basis for your health, longevity, or performance?
[Garth Nicolson]: Well of course we look routinely at membrane lipids, for example, in our blood. We look at things like homocysteine and so on – and my levels are very low. I find that I feel better on NT Factor and, by the way, I have gone on a trip recently and I forgot to take it along, and I suffered because of it.
[Damien Blenkinsopp]: Oh no.
[Garth Nicolson ]: I feel very strongly about taking it on a daily basis. So I’ve seen it in myself. I mean I know that I can recover much faster from travel associated problems, for example, from illnesses and so on and so forth if I take the NT Factor.
And that’s what other people reported back to us as well, it’s not just my own personal results. We get a lot of feedback from a lot of people who are taking this, and now tens of millions of doses have been given to patients and subjects and so on, in various forms, and so far we haven’t had any complaints. And that’s a good news.
[Damien Blenkinsopp]: Its great news, it’s amazing news. Thank you very much for your time today, Garth. Its been great to have you on the show.
[Garth Nicolson]: Sure. Thanks for having me.