This episode presents an in depth look at heart disease because this is one of the most likely things to shorten our lifespan. We focus on the key topic of quantifying your real heart disease risk.
One in three deaths in the United States are caused by cardiovascular disease. Even worse, one of out two Americans will suffer some form of heart issues, meaning that one half of the population is at risk. The total costs for dealing with heart disease are larger than any other disease by far, estimated at 650 billion dollars in the US.
While heart disease is a big risk which is worthwhile taking a look at, it is not a big risk for everyone. For some people there are other health risks they should look at and assess. Thus it is important to know if heart disease is something you personally need to act on – in a proactive way which reduces the risk for it. Are there specific factors you need to be concerned about?
The way to approach this issue is by quantifying our risk for cardiovascular disease. Naturally, understanding of risk goes beyond the typical cholesterol numbers. We discussed some of the problems with cholesterol biomarkers in Episode Seven with Jimmy Moore which is a useful preamble to this episode. In this show we go deeper into details, looking at metrics which give you a real accurate view of your heart disease status and risk.
“There is a way to be very accurate, both [by] blood work and by imaging. To really nail down your personal risk of experiencing the number one killer in the Western world, heart disease.“
– Dr. Joel Kahn

Joel Kahn has focused his career on preempting cardiovascular and heart disease. His goal is to reduce risks as well as to avoid surgery and cholesterol – lowering drugs. He takes a proactive approach by using information and interventions to ensure that heart disease does not become a problem in patients.
He is a clinical professor of medicine at Wayne State University School of Medicine, and Director of Cardiac Wellness, Michigan Healthcare Professionals P.C. He is a Summa Cum Laude graduate of the University of Michigan School of Medicine and author of two books, The Whole Heart Solution and Dead Execs Don’t Get Bonuses: The Ultimate Guide to Survive Your Career With a Healthy Heart.
Joel has also recently set up the Kahn Center for Cardiac Longevity. In their institution they emphasize early imaging of arteries and extensive laboratory evaluation for the correctable root causes of heart disease. So Joel and his clinic have a very quantified and longevity focused approach to this whole area, which is great to see.
I think this is an episode everyone should listen to, because absolutely everyone is going to have to deal with these issues in their life. Inevitably everyone comes into contact with heart disease, whether it be through themselves, their family, or their friends.
The episode highlights, biomarkers, and links to the apps, devices and labs and everything else mentioned are below. I’d love to hear what you think of the episode – and if it has helped you – let me know in the comments!
What You’ll Learn
- What led Dr. Kahn to choose a career in cardiology (4:30) .
- A holistic view of the true causes behind developing heart disease (6:17) .
- The causes behind heart attacks and strokes are tightly related and how both conditions are preventable (9:05).
- How the condition of the endothelium (inner wall of blood vessels) and mitochondria affect cardiac health (10:26).
- The biomarkers Dr. Kahn uses in his practice and ways to personalize medical and lifestyle advice (15:08).
- Infrared Sauna treatment is proven to have positive effects on cardiovascular disease treatment (23:27).
- Using chelation in treating disease to lower toxins levels – including heavy metals (26:03).
- Early detection of coronary artery plaque using a CAT-scan for coronary artery calcium (30:47).
- Because CAT scans are radioactive an ultrasound-based carotid IMT test is used for following disease progression (37:09).
- How to get informed and decide whether to get a coronary calcium test (39:24).
- Understanding genetic testing results in conjunction with imaging of arteries (41:04).
- The Liposcience NMR technology platform offers the most accurate measurement of LDL cholesterol particle density (43:35).
- Familial genetics and lifestyle when tracking lipoprotein levels as a biomarker for cardiovascular disease risk (44:07).
- Using C- Reactive Protein (CRP) as a biomarker for cardiovascular disease risk (46:36).
- Measuring blood vessels inflammation as part of a comprehensive heart health assessment (48:04).
- Diet recommendations for preventing heart disease and examples of successful programs (50:00).
- Replacing dairy products with healthy hydration is beneficial but strict ketogenic diets exhibit negative health effects by causing adrenal stress (54:19).
- Why dark coffee is generally a health drink and the caveats to consider when consuming coffee (59:00).
- Scientific and medical practice sources for discovering topics in this episode (1:01:32).
- The biomarkers Dr. Joel Kahn tracks on a routine basis to monitor and improve his health, longevity and performance (1:03:50).
Thank Dr. Joel Kahn on Twitter for this interview.
Click Here to let him know you enjoyed the show!
Dr. Joel Kahn & The Kahn Center for Cardiac Longevity
- Dr. Kahn’s Web Page
- Dr. Kahn’s Career Biography
- The Kahn Center for Cardiac Longevity: Founded by Dr. Kahn with the aim of preventing heart disease.
- Dr. Joel Kahn Research: PubMed search for Dr. Joel Kahn.
Books by Dr. Kahn
- The Whole Heart Solution: Halt Heart Disease Now with the Best Alternative and Traditional Medicine
- Dead Execs Don’t Get Bonuses: The Ultimate Guide to Survive Your Career With A Healthy Heart
Tools & Tactics
Interventions
- Far Infrared Sauna: Sauna treatment improves heart health, especially in patients who have suffered heart attacks or have blocked arteries. As Dr. Kahn claims, repeated treatment consisting of 15 minutes infra-red sauna followed by 30 min rest helps the body sweat-out toxins and improves cardiovascular system function (See study looking at use of infrared sauna therapy for heart patients).
- Chelation: Chelation therapy has been scientifically proven to rid the body of excess of toxic metals and is approved by the FDA for this purpose. This published study summarizes the findings of the US National Institute of Health clinical trial – specifically on using intravenous EDTA chelation therapy for coronary heart disease. We covered chelation and removing metals in greater depth in past episodes: episode 13 with Chris Shade (Mercury) and episode 19 with Garry Gordon.
Supplementation
- EDTA: EthyleneDiamineTetraacetic Acid is the main chelating supplement discussed in this episode, and which is supported by the studies, in particular to chelate lead.
- Niacin: Also known as vitamin B3 – is an essential human micronutrient. Supplemental niacin is primarily used to treat high cholesterol. Dr. Kahn claims that niacin is particularly good at lowering lipoprotein(a) levels – a proven risk factor for cardiovascular disease.
- Proline / Lysine: Dr. Kahn claims that intake of these amino acids may prevent the damage that lipoprotein(a) otherwise imposes on the cardiovascular system.
- Coenzyme Q10 (CoQ10): Helps support healthy mitochondria in cells. In turn, this maintains a robust cardiovascular system. Dr. Kahn encourages most of his patients to take this supplement.
- Vitamin C / Liposomal Vitamin C: Proponents of the Pauling Therapy from Linus Pauling argue that heart disease can be treated, and even cured, by substantially increasing Vitamin C intake.
Diet & Nutrition
- Nitric Oxide (NO) Supporting Foods (Watermelon, Hemp Seeds, Pine Nuts etc.): Nitric Oxide (NO) is synthesized by the inner walls of blood vessels – known as the endothelium. It prevents arteries from constricting or spasming. NO prevents heart attacks in both an immediate and a long term time frame. Dr. Kahn suggests foods which support NO synthesis including watermelon, hemp seeds and pine nuts.
- Coffee: As a drink, coffee is a rich source of beneficial antioxidants. However, it’s positive effects may depend in part on what type of caffeine metabolizer you are. If you metabolize caffeine slowly then you have a tendency to feel jittery or racing heart and there is some evidence that it may be less heart healthy than for fast metabolizers of caffeine. However, overall caffeine is considered a health food in most studies, and Dr. Kahn recommends 1 cup of black coffee per day to his heart patients.
- Tea: The intake of tea is also an advisable health practice including green tea, herbal tea, hibiscus tea, or chamomile tea before bed – which is a source of sleep support.
- Vegetarian / Vegan Diets: A vegetarian diet excludes meat by focusing on plants for food, but may include animal products such as milk and eggs. In addition to excluding all meat products, a vegan diet also excludes all animal products. Dr. Kahn argues that in world areas where people live the longest, and with the greatest freedom from heart disease, the populations are not completely vegan.
- Paleo: This diet is based on the foods that paleolithic humans might likely have eaten. It includes meat, nuts, and berries, and excludes relatively – recently developed food products including animal products such as milk. Dr. Kahn described his view that there is a lack of scientific evidence to support this diet for cardiac health.
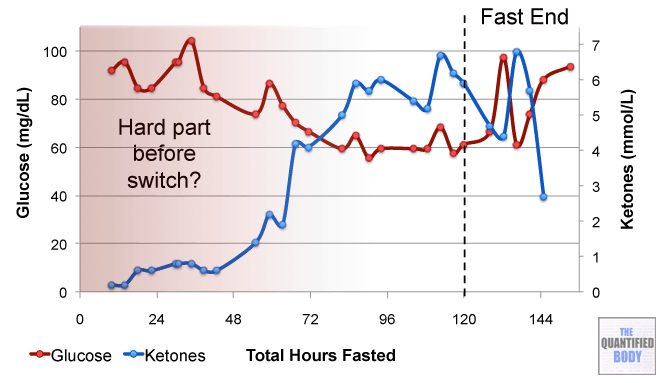
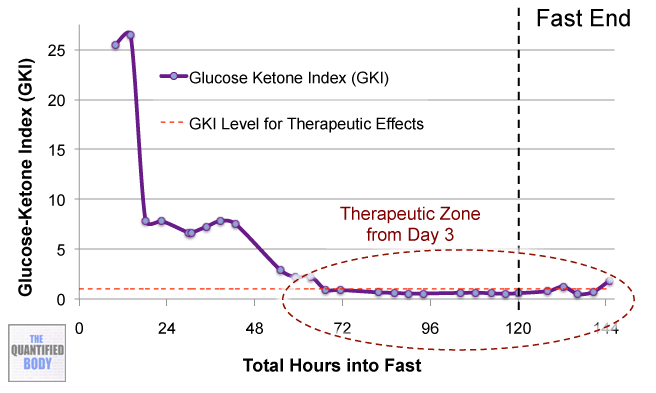
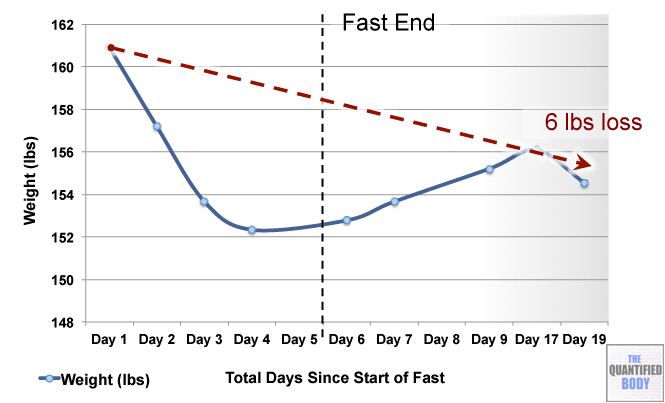
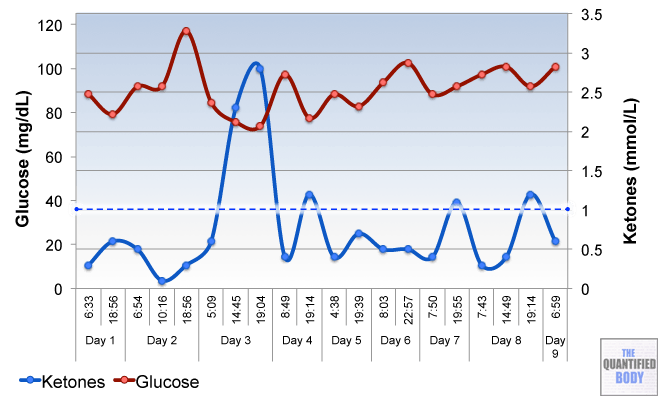
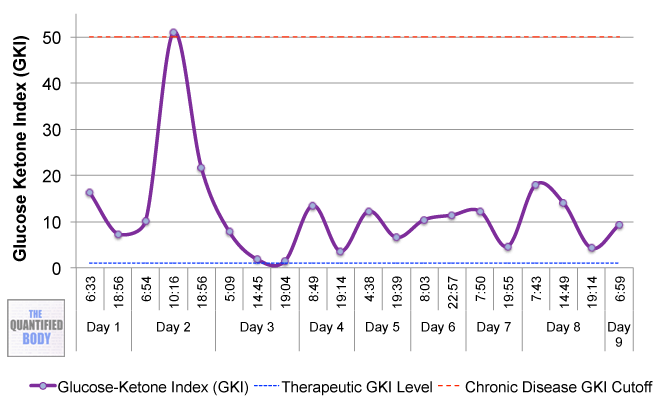
- Ketogenic: A ketogenic diet is a diet that induces a state of ketosis in the body where the body uses ketones instead of glucose for fuel. Typically this involves a diet with low carb and low to moderate protein intake with high fat intake. Previously, we discussed measuring ketones and ketogenic dieting in Episode 7 with Jimmy Moore.
Tracking
Biomarkers
Cholesterol Based
- High – Density Lipoprotein (HDL): The traditional measure of ‘good cholesterol’ used by doctors and healthcare. Levels above 60 mg/dL are considered protective of cardiovascular disease. Dr. Kahn stresses the importance of checking your cholesterol, even at around the age 18 or 20.
- Low Density Lipoprotein (LDL): The traditional measure of ‘bad cholesterol’ – the type which causes heart disease. Less than 100 mg/dL is considered an optimal level, while levels between 160-189 mg/dL increase the risk for cardiovascular disease. Research has shown that LDL alone is not the best predictor for cardiovascular risk. Actually, LDL particles with the smallest sizes are most damaging to the cardiovascular system. Dr. Kahn puts more emphasis on using the LDL particle number and LDL particle size metrics.
- Lipoprotein(a): Lipoprotein molecules carry cholesterol and similar substances through the blood. A test can be done to measure a specific type of lipoprotein called lipoprotein-a. Higher levels of this marker are associated with risk of artery damage. Dr. Kahn states that in most labs normal reference ranges for lipoprotein(a) should be under 30 mg/dL.
Blood Sugar Regulation Markers
- Fasting Glucose Levels: A biomarker used to understand blood sugar regulation. Optimum levels are between 70 and 90 mg/dL. Higher levels indicate some level of blood sugar dysregulation, which increases risk for diabetes II.
- Hemoglobin A1C: A form of hemoglobin which is measured to identify the average plasma glucose concentration over prolonged periods. Higher levels of hemoglobin (A1C) indicate poorer control of blood glucose levels. In turn, these are associated with diabetes and cardiovascular disease risk. Normal levels are less than 5.7%, pre-diabetes levels range between 5.7 to 6.4%, while higher than 6.4% is indicative of diabetes.
Inflammation Markers
- High Sensitivity C-Reactive Protein (hs-CRP): Elevated hs-CRP levels indicate inflammation which is damaging to inner artery walls. If your level is below 1 mg/L then you do not have a cardiovascular disease risk. Because of the proven clinical use of this biomarker, Dr. Kahn claims it is high time for cardiovascular patients to start measuring hs-CRP.
- Homocysteine: Elevated homocysteine blood levels indicate blood vessel inflammation and higher risk for coronary artery disease. This marker has previously been discussed in episode 5 with Ben Lynch and in episode 29 with Dr. Nicolson.
- Lipoprotein-associated phospholipase A2 (Lp-PLA2): This biomarker gives insight into inflammation of blood vessel walls and is useful as part of a comprehensive assessment. The PLAC test measures the activity of ALp-PLA2 (an enzyme) in a patient’s blood. Individuals with test results showing Lp-PLA2 activity greater than 225 nmol/min/mL are at increased risk for cardiovascular disease.
Other
- Ferritin: Serum ferritin acts as a buffer against iron deficiency and iron overload. Levels are measured in medical laboratories as part of the workup for detecting iron-deficiency anemia. The ferritin levels measured usually have a direct correlation with the total amount of iron stored in the body. Female normal reference range is 12-150 ng/mL and for males it is 12-300 ng/mL.
- Myeloperoxidase: A very sensitive biomarker for predicting myocardial infarction in patients with chest pain. It shows added predictive value compared to measuring hs-CRP alone.
- Vitamin D: A vitamin which is essential for bone development and maturation and prevents osteoporosis. The Vitamin D Council suggests an optimum level of 50 ng/mL. The 25-hydroxy Vitamin D Blood Test is the most accurate way to measure how much vitamin D is bioavailable to be used by your body.
- Free Testosterone: A steroid sex hormone. Physiological effects include muscle growth, increased bone density, and development of male sex characteristics. Free Testosterone is a small portion of this hormone which is bioavailable, because it remains unbound by carrier proteins in the bloodstream. Free testosterone reference ranges for females are 1.0-8.5 pg/mL and 50 – 210.3 pg/mL for males.
- Estradiol: This is the primary female sex hormone. For females, the levels of this hormone vary greatly because of its key role in regulating menstrual cycles. In the normal reproductive cycle, estradiol levels measure typically <50 pg/ml at menstruation, rise with follicular development (peak: 200 pg/ml), drop briefly at ovulation, and rise again during the luteal phase for a second peak. At the end of the luteal phase, estradiol levels drop to menstrual levels unless there is a pregnancy. The reference range for healthy adult males is 14-55 pg/mL.
Lab Tests, Devices and Apps
- Coronary Artery Calcium Score (CASC) Test: This test is a type of CAT scan which determines whether your arteries contain clotting plagues by quantifying calcium presence. By measuring calcium scores, the extent of blocking can be determined. This test lasts very short (under a minute), does not require injections, and is not claustrophobic. CASC tests have been shown to predict mortality.
- Carotid Intima-Media Thickness (IMT) Test: This test measures the thickness of the walls of your arteries and helps determine whether you have a higher risk for cardiovascular disease. Individuals with unwanted CASC Test scores should undergo IMT ultrasound as a follow up for disease progression or risk. This is because the CASC test is based on a x-ray CAT scan, as opposed to the harmless ultrasound waves used in the IMT test.
- WellnessFX Cardio Lipoprotein Profile: This test panel includes a number of lab tests, including the comprehensive analysis of lipoprotein particle numbers and sizes. It uses the accurate direct-measurement laboratory method (NMR (Nuclear Magentic Resonance) lipoprofile). Individuals with patterns of higher counts of smaller particles have a more concerning lipoprotein profile than those with less particles with greater size.
- Life Extension Company Blood Testing: Joel mentioned LEF as one of the organizations that provides direct to consumer blood testing that he trusts.
- Caffeine Metabolism Genetics: Whether you metabolize caffeine more rapidly or slowly depends on the presence of a Single Nucleotide Polymorphism (SNP) genetic variation in the liver enzyme responsible for metabolizing caffeine. The company 23andMe offers a genetic test for identifying slow metabolizes who may be at increased risk for cardiac attack due to coffee consumption.
- Toxin Concentrations: These can be measured using blood or urine tests available in specialized labs. We’ve covered this subject extensively in previous episodes – see episode 13 with Chris Shade (Mercury), episode 19 with Garry Gordon (Lead) and episode 23 with Kara Fitzgerald (other metals and chemicals).
Other People, Books & Resources
People
- Dr. David Katz: Founding director of Yale University’s Yale-Griffin Prevention Research Center and current President of the American College of Lifestyle Medicine.
- Tim Russert and James Gandolfini: Both men were prominent individuals in American culture, whose lives were shortened by sudden unexpected cardiac attacks.
- Linus Pauling: An American biochemist, author, and educator as well as one of only four individuals to have won the Nobel Prize twice. During the 1990s Pauling put forward a plan for the treatment of heart disease using vitamin C.
- Stormie Jones: Was the world’s first recipient of a successful simultaneous heart and liver organ transplant at the age of six. She suffered from an inherited genetic condition named Heterozygous Familial Hyperlipidemia which made her liver unable to remove cholesterol from her bloodstream. In turn, this was also causing her serious heart problems.
- Nathan Pritikin: An American inventor, nutritionist and longevity researcher. His program features the Pritikin Diet which is focused on a variety of whole (unprocessed) or minimally processed foods.
- Dr. Dean Ornish: A cardiologist and the founder of the non-profit Preventive Medicine Research Institute. He coaches patients towards a vegetarian diet but not a strict vegan diet. His program is defined in four specific elements of lifestyle. It is the first scientifically proven program to “undo” (reverse) heart disease by optimizing stress, diet, physical activity, and social support.
- Dr. Caldwell Esselstyn: His proposed diet for cardiac health is strictly vegan with under 10 percent of calories coming from fats. His program for patients includes walking, meditation, stress management, yoga, and other lifestyle choices to decrease cardiovascular disease burden.
- Dr. Neal Barnard: An associate professor of medicine at the George Washington University School of Medicine. He has led numerous research studies investigating the effects of diet on diabetes, body weight, and chronic pain.
- Dr. Garth Davis: Among the leading researchers in the field of bariatric medicine – a branch which deals with the causes, prevention, and treatment of obesity.
- Dr. William Davis: A cardiologist and author of the Wheat Belly blog.
- Dr. David Perlmutter: A Board-Certified Neurologist and Fellow of the American College of Nutrition.
- Dr. Alessio Fasano: An Italian researcher who sees pediatric and adult patients in the Center for Celiac Research and Treatment at the Massachusetts General Hospital. He is carrying out important research on the health impact of eating grains.
Organizations
- Wayne State University School of Medicine: Where Dr. Kahn is a clinical professor.
- Michigan Healthcare Professionals: Where Dr. Kahn is Director of Cardiac Wellness.
- University of Michigan School of Medicine: From where Dr. Kahn graduated with a Summa Cum Laude degree.
- American College of Cardiology: Mentioned by our guest because the ACC have given a high endorsement of the CASC test for people with cardiac risk factors.
- The Harvard School of Public Health: Mentioned by Dr. Kahn as an important institution in support of minimizing dairy intake. Dairy products should be replaced with healthy hydration such as water, teas, coffee (unsweetened) and even alcoholic drinks to a limited degree.
- Life Extension Company Blood Testing: Joel mentioned LEF as one of the organizations that provides direct to consumer blood testing that he trusts.
Books and Video
- Wheat Belly: Lose the Wheat, Lose the Weight, and Find Your Path Back to Health: Written by William Davis whose books Dr. Kahn recommends reading.
- Grain Brain: The Surprising Truth about Wheat, Carbs, and Sugar-Your Brain’s Silent Killers: Written by David Perlmutter whose books Dr. Kahn also recommends reading.
- Forks Over Knives – A Film That Could Save Your Life: A film by director Lee Fulkerson which examines how disease can be reversed by rejecting our present menu of animal-based and processed foods.
- The Widowmaker: A documentary on the topic of coronary artery calcium score (CASC) testing. It explains why CASC testing is not more available in the American healthcare system.
Full Interview Transcript
[04:30][Damien Blenkinsopp]: Joel, thank you so much for coming on the show.
[Joel Kahn]: My complete pleasure.
[Damien Blenkinsopp]: So, I’d like to start with a quick story about how you became a cardiologist; why did you get into, specifically, holistic cardiology?
[Joel Kahn]: Sure.
I knew really from a very young age that I wanted to be a cardiologist. I actually had a very small issue as a young child with a tiny hole in my heart. It healed, but I had the pleasure of seeing a very fine heart doctor until I was about 18 years old.
It had a very good impression on me; [there were] a few scary moments being in a big hospital as a little kid, but overall it was actually very positive. And kind of pursued a fast tract to making this my career. I’ve been doing it now for almost 26 years after training.
Holistic? I just always felt people are more than a pill. Doctors are wonderful people, nurses are wonderful people; I don’t have a chip on any shoulder. But I was exposed to some really good people. I got very involved in nutrition, nutrition lead to Mind Body, nutrition lead to Standard and Alternative Fitness, nutrition lead to supplements, Yoga, meditations.
So I just poured my heart and soul into studying and learning, and expanding my tool box for patients. And then I said, I’m going to start writing about it, because I don’t know if [they] are practicing it. So it’s all been a wonderful journey that’s far from over.
[Damien Blenkinsopp]: I didn’t realize you’d had that heart issue. Is it completely resolved now?
[Joel Kahn]: Yeah. Yeah. It’s very common, a little worrisome to the parents — god bless my mother and father. But it’s another example of if you don’t get in the way of things, the body can often heal itself. And this was a relatively minor thing, so good for that.
[Damien Blenkinsopp]: Great to hear. And it gave you the motivation to get started in all of this. It’s kind of funny who life always does that; it kind of steers us in the direction we end up going.
[06:17] I was wondering, because you’ve been looking at this holistically — and a lot of people focus on the heart, cholesterol, and things like this — could you explain what a formula to get heart disease would be, in terms of a holistic view? Because when you read through your book, it gives you a much more global view of how heart disease comes about than we’re typically used to.
[Joel Kahn]: Yes. And you know, we don’t want to throw away the basics. In essence, there’s two ways to approach this.
Our government, the United States government, has been publishing for a while, every 10 years, major causes of death. And unfortunately heart disease is at the top of that list, every list, every 10 years. But that’s not really the true causes, and starting in 1993 some very open-minded researchers said, “Let’s talk about the true causes.”
And the true causes for 80 to 85 percent of premature deaths were three activities: smoking, poor fitness, and poor diet. And those true causes dwarfed everything else. And it always dwarfed genetics. It’s a lifestyle world, baby, in terms of developing or preventing heart disease.
So, heart disease develops because we smoke too much; fortunately, under 20 percent of the population, and it used to be 40 to 50, so major inroads, it’s falling. Heart disease develops because we don’t move enough, and we’ve gone from farming and active community 150 years ago to everything being tech based, and we’re blessed with all of that. But we are paying a price.
And we now have to use, I have an app on my phone that reminds me to stand 5 minutes every hour. So we’ve come full circle, where technology was the problem and now technology will provide solutions. And desks that go up and down so you can stand at work and such.
And then heart disease develops because of the change in our diet since the Golden Arches hit California in the 50s, and all that’s followed with giant companies and processed food, and our crazy lifestyle where we don’t have time to make meals from whole foods anymore. Those are the big three by far.
A good friend at Yale, head of Preventative Medicine Dr. David Katz says, “Forks, fingers, feet.” Fork, what you do with it will determine your life; fingers what you do in terms of smoking, and feet whether you move and exercise that body. And really that accounts for the majority of it.
Sleep, stress, and love would be the other three. Adequate sleep, managing stress, and including yourself in a community to be surrounded by loving, like-minded people would round out the top six. And that’s a pretty holistic view, but it’s not very difficult, and it’s not very sophisticated.
[Damien Blenkinsopp]: Yeah, great, thank you very much for that.
[09:05] And I think when we think about heart diseases we often think about heart attacks, but is stroke related to heart disease as well? Is that one of the outcomes from the same kind of mechanism?
[Joel Kahn]: Yes. Stroke is a little bit more diffuse or widespread in terms of trying to nail down the cause. The number one listed cause of death in the United States is heart disease, such as heart attack. And number three is stroke, with cancer between the two. Therefore, if you lump heart disease and stroke, cardiovascular disease is the number one cause of death in every segment of the population over age 30, men and women.
But stroke has a shared cause to heart attacks; that is you can get clogged arteries from the lifestyle measures, and in part genetics that I just ran through. But there are other causes of stroke: bleeding disorders, heart rhythm disorders.
So the data is you can prevent about 80-90 percent of heart attacks through adopting a healthy lifestyle that’s neither expensive nor difficult, just rarely done. And you probably can prevent about 60 percent of strokes. It’s not as high because the cause is more commonly something other than atherosclerosis, or hardening of the arteries.
[Damien Blenkinsopp]: Great, thank you for that. Yeah, because I wasn’t really aware that they were so tightly related and preventable as well.
[10:26] In terms of stressors and some of the other mechanisms, could you talk a bit about the actual mechanisms behind heart disease? How this takes place? Without getting, obviously, into crazy detail, because it can get pretty detailed.
But in your book you talk about a variety of factors that we don’t often think about, such as mitochondria, and the gut, and other areas. And we don’t think about those leading to heart disease. So could you give us some kind of overview to show us how these mechanics are working to create a condition.
[Joel Kahn]: Well certainly, and one term that readers and listeners may not be familiar with but is important to grasp is something called your endothelium. And that is, essentially, inside every artery in your body — miles and miles of arteries carrying blood to your brain, your pelvis, your heart, your organs, your toes — is a one cell layer thin lining, like wallpaper on a wall.
And until about the 1980s we thought it was simply just a cell barrier between blood on the inside and the structure of the wall on the outside. But now we know that the endothelium makes many chemicals, the most important of which, or perhaps the most crucial, is nitric oxide, a little simple gas that in a healthy artery is created in abundance.
Arteries making nitric oxide because of a health endothelium will resist the clotting of blood; you want the clotting of blood when you cut your finger, you don’t want the clotting of blood when you’re on the verge of a heart attack. The nitric oxide will prevent; arteries from constricting, or spasming, which again can trigger a heart attack; the Raynaud’s blue-white-red fingers some people struggle with in the cold; leg pain on walking; and also the actual plaque, the actual build up of debris in arteries is resisted by a healthy endothelium with healthy production of nitric oxide.
So, that’s one physiology, and the good news is things that we would associate with a healthy lifestyle –eating a lot of produce, fresh fruits and vegetables, exercising your body, adequate sleep, good blood pressure, good blood sugar, good cholesterol numbers from a healthy lifestyle — are all associated with a healthy endothelium. And if you have a sick endothelium, you can make it healthier though a healthy lifestyle.
All of these things resoundingly shown scientifically. For example, eating watermelon, [it’s] very rich in chemicals that support nitric oxide. Hemp seed [is] very rich in chemicals that support nitric oxide. Other seeds and nuts similarly: pine nuts.
The other one [is] as you mentioned; inside every cell are little organelles, or little structures inside our cells. We have trillions of cells —- brain, heart, muscle, everywhere — and their powerhouse to generate function is called your mitochondria. We don’t think about them, we don’t give our mitochondria a kind of shout-out, we don’t wake up in the morning and say, “Thank you mitochondria for taking care of me while I slept seven and a half hours.”
But indeed, aging is a stress on our mitochondria where they won’t function to make energy so well. And unfortunately we now know not only bad lifestyle, which is way too common — sedentary lifestyle, food-based poor lifestyle, smoking poor lifestyle — but environmental toxins clearly affect our mitochondria: pesticides, herbicides. There’s data that genetically modified products and the herbicide roundup affects our mitochondria. Nutritional deficiency like low magnesium from not eating enough produce affects your mitochondria.
And our cells will age quicker and won’t function as well, and may produce fatigue, may produce congestive heart failure, shortness of breath. But again [it is] an area of science that is very hopeful, because lifestyle can cause our mitochondria to be much more efficient, and, probably most strongly, exercise. The actual number and health of your mitochondria in your muscles goes up when you exercise. You actually, you can be in your 40s and 50s and you can create more mitochondria by regularly exercising to a fairly vigorous degree for a while.
So yeah, those are concepts that I think are important to share. And there’s ways to boost the function of both our endothelium and our mitochondria, both by lifestyle, and not — I’m a fan of selected supplements. The supplement Co-enzymeQ10, CoQ10, which is more commonly used in Europe than the United States, helps support healthy mitochondria and [it’s] something I encourage most of my patients to be on.
[15:08][Damien Blenkinsopp]: Great. So, on this show we talk about a lot of biomarkers, and I know you have preferences for different biomarkers from the standard.
Could you, first of all, walk us through some of the very typical. I mean, when most people go to their doctor they are given the standard cholesterol markers. So could you talk through the LDL, the HDL, the total cholesterol, and if you use those, and how useful you find them.
[Joel Kahn]: First step, and I always like basics, is get your cholesterol checked, even at around age 18 or 20. Because one out of every 400 people may have an inherited disorder called Heterozygous Familial Hyperlipidemia, or FH, and you may be 18 years old with a cholesterol 450.
One out of every 400 is not all that rare. In a typical high school in this state that might be six kids. And it’s better to know it at age 18 or 17 than to find out in an emergency room at age 45 with a heart problem.
But in my practice, I do advanced cholesterol lab values. There’s a variety of different ways. For example I can see two people with a cholesterol of 220 and the LDL cholesterol of 120, and they may be at very different risk for artery damage because we can break down the size of their LDL, the number of particles in their LDL. Usually it’s a technology called NMR spectroscopy, but it’s become a very low cost lab that’s much more accurate.
So I can have two people and I can speak to them differently; that’s called personalized medicine. And say, “Nancy, your LDL is actually very favorable. You don’t have much. They’re large particles, and I think we can leave you alone and continue your good lifestyle. And Joe, your LDL of 120 is constructed largely of small, dense particles, and you’ve got way too many of them. And we’ve got to really kick that lifestyle in gear, and your nutrition in gear, and we’ve got to get that belly a little thinner.”
You know, it can help me define a more guided approach. But when we’re talking population, a standard finger prick or church-based or work-based cholesterol is a good starting point.
[Damien Blenkinsopp]: Right. It’s just a screen to see if it’s worth digging further. So basically, if LDL comes up high, you’d be like, okay I’ll look at the particle number and size to see if this is a problem.
[Joel Kahn]: It can. Yes, that’s one of the things we can do to refine if, everybody needs encouragement about lifestyle, but if they need beyond that consideration of medication or more intense lifestyle.
[Damien Blenkinsopp]: Great. So is it possible for someone to have a high LDL number, which is over the standard reference range, and it not be a problem because the size of their particles is large and small number of particles, basically?
[Joel Kahn]: Yeah. We broke up a little, but cholesterol is associated with developing heart disease. And it is causative, there’s no doubt. I mean, I reflect back when I was in cardiology training in Dallas, Texas.
I took care of a little girl, 11 years old, who was known around the world, Stormie Jones was her name, sweet girl. And she was born with a genetic disorder where she had both genes defective, that was called Homozygous FH. It’s very rare, it’s about one person in a million. But that little girl had had a heart attack, a bypass, a balloon, by the age of 12. And to argue that cholesterol doesn’t have a direct role in damaging arteries has many pieces of science behind it, animal and human, but I always reflect back on Stormie Jones.
So cholesterol is important, but there’s so much variability in human physiology. So when I’m dealing with one person, I try to find if their arteries are healthy or not. There are ways to determine if there’s any early plaque, if there’s any early endothelial damage.
And if I see somebody with a fairly high cholesterol at age 60, for example, but they have no evidence of plaque, no evidence of endothelial damage I’d have a very hard case to put them on a prescription drug, in my mind, because there must be other factors that are protecting them. And yes, they may have an additional 30 or 40 years to worry about, but I’m really going to stress to that person lifestyle — healthy diet, exercise, weight management, blood pressure management — and not necessarily write a prescription drug.
And, you know, there’s always the opposite too. There are people that have had a heart attack, or a bypass, and relatively moderate risk factors, and then we really have to go on a search. We have to go on a search for other biomarkers, like something called Homocystine, lipoprotien(a), Ferritin.
There’s a lot of people that are prediabetic that fall through the cracks, and are suffering artery damage from their prediabetes, but it’s really not been offered as a diagnosis, and that’s kind of a very common one, for example.
[Damien Blenkinsopp]: Right. With the Homocystine, for example, are you looking for the causes? Or are you trying to look a bit further back?
So if you get some high cholesterol numbers and some particle numbers that are indicative, is homocystine more indicative of a cause, so you can refine your prescription, the treatment you recommend? Or is that just a basic filter for your assessment?
[Joel Kahn]: No, I think the ultimate joy is trying to get back to the root cause. And the root cause, certainly the majority of it, is lifestyle. And we’ve talked about that, food choices, which I’ll go over carefully with patients: processed versus unprocessed, high in saturated fat versus low, high in added sugar versus low. [And also] body movement, body fitness, body exercise, adequate sleep, methods of managing stress.
For example, it’s been shown that meditation can have a significant effect on lowering your cholesterol. Kind of pieces of scientific data that are published that aren’t talked about much. When you’re stressed out your cortisol level goes up, your blood sugar goes up, your blood cholesterol goes up, your blood pressure goes up. And a practice of breathing or yoga or meditation can fairly dramatically lower blood cholesterol.
So then getting at the root cause, now the question is after those basics, which need to be addressed every visit, over and over — sleep, stress, nutrition, fitness — do we go further? We do know that there are environmental toxins, and we do know that heavy metals we’re exposed to through cosmetics, through industrial exposure, through dental fillings. We often carry a burden of mercury and lead and cadmium.
Smokers not only are ingesting all kinds of toxic carcinogens, but the ground in Virginia is said to be quite rich in cadmium, which is fine if you have it in the battery that’s powering your radio but you don’t really want cadmium in your blood stream in your body. So you can use blood analysis, hair analysis — take a little snip of hair — or urine analysis and determine if a person has greatly elevated levels of some of the pesticides, herbicides, pollutants like heavy metals.
And sometimes the course directed at identifying and removing those can really restore a person’s health to a much higher level. It’s a slow process because you accumulate those things slowly, and any plan to exit them by avoiding; if it’s an industrial exposure taking more care or changing jobs, don’t walk on your lawn the day that they spray the pesticides or look for more natural organic way to treat your lawn. Consider whether your mercury in your mouth might be a problem or not, you can get tested for that, for example. All those things.
But then there are strategies to remove some of these toxins. And of course considering eating organic versus non-organic to lower our input of pesticides. These are all strategies; and then there are more advanced strategies.
I’m a big fan based on some very fascinating and rich scientific data of the health benefits of sauna on our overall health, and specifically our heart health. And the amount of data that supports it is surprisingly rich, but very rarely taught in the annuls of medicine, of course.
[23:37][Damien Blenkinsopp]: Is that any type of sauna, or is that the infra-red version?
[Joel Kahn]: Well the infra-red is the hottest and most widely mentioned, because in Japan, starting about 20 years ago, heart patients have been treated, heart patients who’ve had a heart attack, heart patients who’ve had blocked arteries or even the very serious problem called congestive heart failure, have been treated with 15 minutes of infra-red sauna followed by 30 minutes of rest and it has been shown that they can enjoy dramatic improvements in health.
And these are all actually published studies; scientific journals, some of them involving up to about 200 patients, which is getting to be respectable size for a research project at all. So that’s infra-red sauna, which is a special kind of deeply penetrating heated dry sauna; not that common in this country at this point. People can consider buying one for their home for under $1000 up to a few thousand, or finding a spa that might have an infra-red sauna, which is growing interest in this country.
But recently, as you may be aware, out of thin [24:50 unclear] came a large research study with 2000 people that were asked how often do you get in a sauna, how long do you sit in a sauna, and all that tracked with actually survival and heart health. And the number of days a week that people used sauna, and the number of minutes per sessions were kind of linearly related to overall health, which was large, and shocking, and made the news. And that’s a slightly different form of sauna. It was dry sauna but not infra-red.
So I think there’s much hope in perusing that. And the theory is that it may have something to do with detoxification. There’s no doubt that the sweat that is generated in such a thing as infra-red sauna is rich in heavy metals, richer than your urine or richer than your blood. You’re actually exiting these toxins from your body in your sweat.
So I’m a big fan of that. Then you can get into other approaches, so called oral chelation, juicing, using green vegetables like broccoli, sprouts, oregano, parsley and other greens to accelerate the exit of some of these toxins from your body in a fairly easy and natural way.
[26:03][Damien Blenkinsopp]: So it sounds like heavy metals in particular sound like something that you think they are quite relevant and important to heart risk issues.
Did you see, I believe there’s some studies with EDTA and heart disease more specifically and the impacts on it with some of the plaque and things on it. Am I correct in that, have you seen those studies?
[Joel Kahn]: Yeah. I was not a fan of recommending chelation. And so let me just take a step back, because not everybody is going to be familiar with chelation.
But because of industrial exposures to heavy metals in the 40s and the 50s — for example a worker exposed to arsenic in an explosion, or lead — there was an interest in trying to treat those acute toxicities. And various medicines like EDTA have been shown in those kinds of exposures to be quite helpful. And they’re, in fact, approved by the FDA for use in these industrial exposures to heavy metals: heavy lead, cadmium, mercury and such.
But in the process of some of those treatments, there were reports that people with heart disease were describing that they were having less symptoms. And some sharp clinicians were observing this and started to specifically treat some people with clogged arteries of their heart and their legs with chelation. And that, to this day in the United States, is not an FDA approved treatment; you won’t get paid for it, and in your charting you could be subject to some exposure for saying that’s why you’re treating them. Using i.v. EDTA for the reversal of atherosclerosis as opposed to heavy metal toxicity.
So, all of that was kind of subject to derision from the standard medical community, including myself. If you would have asked me four years ago, can we talk about the science behind chelation — I know there’s people that say they feel better, but do we have much science? You would have been very hard put.
So again, very forward thinking people about 10 years ago approached the National Institute of Health and said we need to resolve this; is this witchcraft, is this good care, and let’s do a study. And surprisingly the United States government came up with about 30 million dollars and designed a trial using kind of standard i.v. chelation protocols in, ultimately, 700 people that had survived a heart attack — that’s what was required to be entered in — and they were supposed to show up for about 40 weeks.
Some of them got EDTA based intravenous infusions, some of them got some vitamins, but there was no EDTA in there. And at the end of that study, which took a little longer to complete than hoped, was a little bit more difficult to recruit patients, but the overall trend of the study favored an improvement in outcome, like the combination of being alive, freedom from a heart attack, freedom from needing a bypass and hospitalization in those that got the active chelation.
And specifically two groups, if any of those 1700 people were diabetic or any of those 1700 people had actually experienced a fairly large heart attack in the background in their history, they had a dramatic improvement. It was a 40 percent reduced chance of having a bad outcome. And if you had a pill that within about four to five years reduced those bad events by 40 percent, you’d have a blockbuster new pill.
So chelation looked good, actually, and the combination of i.v. chelation plus potent multivitamins — because that was another aspect of the trial, it’s called the TACT trial, Trial to Assess Chelation Therapy — that the combination of i.v. chelation once a week and potent twice a day multivitamins had the biggest impact. But that was announced, I think it was around November 2012, so more than two years ago.
And there’s really been no movement since to seek out reimbursement, or FDA approval. Most doctors clearly are not set about to offer intravenous therapy. There’s a very small chance of harm. You can lower blood calcium levels because it’s going to chelate minerals, and calcium is one of those so very often the mixture has to have some nutrients and mineral support in it. But I have referred patients to colleagues of mine in the area that are experienced and certified in chelation.
[Damien Blenkinsopp]: Great, great, thank you for that, because the connection is appreciated by a lot of us.
[30:47] So I wanted to look at some of the, because I know you recommend some more accurate tests. For someone who really wants to know for sure their heart disease risk and where it’s at, if the status of their plaques, what do you use to accurately and directly see what the picture is looking like?
[Joel Kahn]: Yeah, well thank you for asking that question, because that’s really my passion. My passion is to teach people that there is a way to be very accurate, both by their blood work — and we talked about that — and by imaging, which we’re going to talk about right now. To really nail down your personal risk of experiencing the number one killer in the Western world, heart disease which can come on suddenly, without warning, and the next day there’s a funeral tragically leaving spouses and children and parents wondering how did nobody pick up that there was a burden of disease.
I’ll just give you a quick example. Sadly a friend of mine lost her husband, who was a prominent businessman in my town, who was a very fit person [who] ate healthy, looked good, wasn’t overweight, enjoyed athletics, and a little over two years ago went out for a bike ride on vacation and never came back. And was found at the side of the road and shown by autopsy to have a 99 percent blocked Widow-maker artery. And that shouldn’t happen.
My passion is to say, that’s tragic and we need to circle around that family with a lot of love, but let’s not let the next family and the next family and the next family, you know the Tim Russerts and James Gandolfini from Sopranos and such. We just had a bank president in my town, about three or four weeks ago, who experienced the same tragic end to his life, a man I’m sure was getting good medical care, absolutely.
So, there is the most accurate way right now to [if] you’re 45, 50, 55 years old, you’re concerned that this this number one killer in America could be creeping up inside silently; And you should be concerned, particularly if you’re overweight or sedentary, or [have] blood pressure, cholesterol, blood sugar issues, smoked in the past, [have a] brother, sister, mom, dad with heart disease.
There’s a CAT scan that takes 10 seconds, 20 seconds. You lie down, you’re pushed into a tube, a CAT scanner. It’s not around your head, it’s not claustrophobic. No i.v., no injection of medication. The CAT scan is done, you go home, you get a report. It’s called a coronary artery calcium scan, or coronary artery calcium score, CACS.
You can see the three heart arteries on the CAT scan without any injection of contrast material. Your arteries should contain no calcium; calcium should be in your bones and your teeth. If your heart arteries have calcium, your heart arteries have plaque. And you’re going to have that way before you ever need to have your bypass, your stint, or your heart attack therapy. So you can find out.
And there’s a number associated with it. If your score comes back zero, you have youthful arteries that are free of calcium, and your 10 to 15 year risk of a heart event are extremely low. Keep living healthy, but you can take a sigh of relief.
And if your arteries are prematurely calcified, you’ve got plaque. You may not be 80 percent blocked, you’re probably not going to need a stint or a bypass, but you need to see somebody about it. So that number could be 20, or 100, or 200.
I get people that show up, I saw one yesterday, totally good looking guy 61 years decent lifestyle, his calcium score was 1,100, mainly in the one artery we call the widow-maker. That’s a ton of burden of abnormal artery that we need to deal with by identifying why, and we’ve talked about some of that search.
He had already had a stress test that was normal, so he doesn’t need an angiogram, stint, or bypass, but now he needs a cardiologist who cares about lifestyle and all of the things we’ve talked about. We talked about yesterday about sauna, and heavy metal assessment, and advanced lipid blood work, and a daily aspirin. He’s a heart patient now, so I plead with people now.
[Damien Blenkinsopp]: Right. Yeah, I guess in that situation you would kind of throw everything at it, because it does sound like you were pointing out the worst case scenario, the worst score you’re likely to see.
Would you kind of throw everything at that case? Should he be really worried, and say, “Whoa, I’ve got to really change my lifestyle. Heavy metal chelation, everything I can.”
[Joel Kahn]: Yeah, that person needs to become a good student of the disease, reading my book, reading a book by Dr. Dean Ornish, a book by Dr. Caldwell Esselstyn. Many many good resources: Dr. Neal Barnard, Dr. David Katz. There’s plenty of good resources online for free, or books, or watch the DVD Forks Over Knives. I mean, many good resources, and I encourage my patients to do all of that.
But we ordered up a pretty in-depth analysis, and we’ll sit down in a few weeks and design a personalized plan. Now on the other hand, I see people all the time, they’re carrying extra weight, their cholesterol is 250, their diet isn’t exactly what I’d called in-line with nutritional goals, and their calcium score is zero at age 65. They’ve gone through six decades of life and are identifying no calcified plaque in their arteries, and their risk is very low.
And I don’t want them going to fast food places and eating their french fries, but I can cut back a bit on their medical treatment and focus on lifestyle with a great sense of joy and relief. And I see that a lot; a brother died at age 44 and the sister is zero and is going to smile for the next few years that she isn’t also carrying a burden of life-threatening plaque.
The oddity about the test is in the United States it’s not covered by insurance in about 48 states; 10 years ago places were charging 700 or 800 dollars. It’s very easy now to find that test under 150 dollars, sometimes under 100 dollars, which makes it very reachable for most people.
[Damien Blenkinsopp]: Is it quite widely available, like a lot of hospitals have these machines?
[Joel Kahn]: It’s just a standard CAT scanner, you do have to have special software to calculate that score, but it’d be very surprising if [in] most medium or large towns at least one of the hospital systems, or all of them, don’t offer it.
[37:09][Damien Blenkinsopp]: Okay. As it’s a CAT scan, is this something you shouldn’t do to often because of the radiation? With your patients, if someone’s got a score of 1000 or above, I guess you’re tracking progress over time to make sure it’s not increasing and you’re reversing some of that damage. But are you concerned at all about radiation, and do you do anything about it?
[Joel Kahn]: Well it’s an excellent question. I am a bit hesitant to repeat the CAT scan to follow their disease for two reasons: every time you do it it is some additional radiation, and number two there is not much data that you can drive that calcium out of the artery.
For example, the TACT trial, the chelation trial didn’t, unfortunately, assess calcium score. It would have been nice if we actually knew. So I don’t know the natural history. I know the natural history tends to go up if you do nothing; there are some studies that your calcium score may go up 30 percent a year. So if your score is 100 this year, it may be 130 next year. That’s just an average; it’ll be less for some, more for some. But I’m not so sure what I’d do with a repeat calcium score, because I fear they all go up.
There is an alternative test, called a Carotid IMT, intima-media thickness. This is an ultrasound. So ultrasound, of course, is no radiation; ultrasound can be repeated. And there’s about 700 medical studies on the value of having a special ultrasound machine with special software, that measures the thickness of the wall of your carotid artery.
And that is something you can track every year, every six months, compared to databases that have thousands of people age matched and sex matched, to make sure your arteries aren’t rapidly getting thicker and more plaque ridden. And hopefully actually seeing some improvement. So, if I have somebody with a bad calcium score, I’m probably going to use an ultrasound technique to follow them so I don’t need to keep exposing them to radiation.
That’s kind of a high level approach, but we’ve got the disease that’s the number one killer in America. So we’re throwing all kinds of high pollutant, expensive technology at other issues, it’s about time and way overdue that we try and prevent a million heart attacks in the next couple of years in this country so families don’t get ripped apart.
[39:24][Damien Blenkinsopp]: Who would you recommend takes the calcium scoring test?
[Joel Kahn]: Thank you for asking that. Not people who know they have heart disease. So if you’ve had a stint, a bypass, if you’ve had a previous angiogram that showed you’ve got 40 percent blockages, you already know you have a problem and you need to be working on it with somebody that can direct you.
However, it would be somebody aged 40 to 45 and up who has risk factors; brother, sister, mom, dad with early heart disease; high blood sugar; high blood pressure; smoker. Or maybe around age 50 to 55 just because you’re halfway through life and you’ve got the number one killer in America lurking around.
The American College of Cardiology, a fairly conservative group, gave very high endorsement of this coronary artery calcium score for people with risk factors. So if you’re 50 years old and you’ve got high blood pressure, boom: American College of Cardiology endorsed, and unfortunately not covered by insurance. They would leave it in a gray zone.
If you’re perfectly healthy 50 year old, do you need it? Well, I think that’s a personal decision between you and your doctor. I tend to favor getting one because it’s a very low dose of radiation and we still are dealing with the biggest silent killer in America.
There’s a very interesting documentary that came out two months ago called The Widowmaker. And it’s available online, about 90 minutes. I’d encourage anybody to watch it. It’s all about this topic of coronary artery calcium scoring and why is it not more available to make inroads into the health of Americans and identify those at risk.
[Damien Blenkinsopp]: Great, great, thank you for that.
[41:04]There are actually a lot of other blood markers. If you look at WellnessFX — I don’t know if you know the WellnessFX lab for consumers?
[Joel Kahn]: Which blood test is that, sir?
[Damien Blenkinsopp]: It’s not a specific blood test, it’s a lab which is directed at consumers. So it’s a company called WellnessFX, and some people are using those for blood panels.
[Joel Kahn]: Right.
[Damien Blenkinsopp]: So they have a large array. There’s a few companies like this, but WellnessFX is the best known at the moment. So it’s direct to consumer. They have a cardiovascular panel, which is why I bring it up. And there’s quite a few things on it.
So I wonder if you could just comment on some of the values that they include in their panel, if you find them useful. Because it seems like to me that there are so many markers linking to cardiovascular disease it makes it more complicated.
Because we have all these markers, and I’m sure someone like you could maybe get more data and get a better picture, but for the majority of us, it builds up this kind of complex mass of data. And maybe some of them would be out of range, some of them aren’t out of range, and we’re like, “Okay, so where does this put me? I’m not really sure.”
[Joel Kahn]: Yeah, I agree. I am familiar with WellnessFX. There are some others — I have no financial ties to any of these. There’s an organization that I very much like called LifeExtension.org. They’ve been in Fort Lauderdale for 35 plus years, and you can directly get a kit and blood work — a male panel, a female panel — and they’ve got hundreds of thousands of data points built up over the decades.
So you’re right, I think it is worth [it]. I have not seen the advanced lab test we talk about, the particle number, particle size. I have not seen that available in a direct consumer way; I’m not absolutely certain if that’s at WellnessFX. But you’re going to get a good screen, and you can learn quite a bit.
But I do go back to the idea that imaging arteries remains the kind of litmus test. You can have a lot of abnormalities in your blood stream, but you really need to know if you’ve either got thickened carotid arteries by the ultrasound, or if you have calcified, hard arteries by the CAT scan. You need to know that at least once to make sense of the blood work.
These biomarkers are all associations, where the imaging studies are direct imaging. So I favor the coronary artery calcium scan. In some places [it] requires a prescription, but since it doesn’t involve insurance, not everywhere, you can often arrange it on your own.
I encourage people to pursue these direct blood tests, like you said.
[Damien Blenkinsopp]: Yeah.
[43:35] I just wanted to go through a couple of them. You mentioned the NMR, which is, as I understand it, the most advanced blood test if you really want to understand your heart disease risk. Is that kind of the best one you find, in terms of accuracy and getting the closest to the same bar as the calcium score, if you’re just looking at blood?
[Joel Kahn]: Yes, in terms of blood, that LDL particle number which is most commonly obtained through the Liposcience NMR technology, is at the present, I believe, still the most accurate particle in the blood you can measure.
[Damien Blenkinsopp]: Yeah, Great.
[44:07] So WellnessFX, they have something called LPa, or lipoprotein(a). Are you up to speed on that one? Do you find that one useful? Because it’s a little bit similar in that it’s looking specifically at low density lipoprotein, I understand.
[Joel Kahn]: Yeah. Lipoprotein(a) is a cholesterol particle that a smaller number of the public has heard about. A very large amount of science saying it’s a blood test, the higher your level, the higher your risk of artery damage. It seems to be a highly inherited abnormality.
So I get it basically in pretty much everybody once, but I’m particularly aggressive in people that have a family history of early heart disease in their relatives, because that may be the factor. Usually in most labs lipoprotein(a) should be under 30, and in some patients of mine it’s over 200; it’s seven, eight, or nine times elevated above normal.
What is still lacking a bit is an absolutely clear cut trial that shows that lowering it — we can talk about lowering it in a minute — but lowering it makes a long term difference, just because there hasn’t been such a trial designed and carried out long term. Lifestyle can lower lipoprotein(a), hormonal balance of female and male hormones can lower lipoprotein(a), Niacin is particularly good at lowering lipoprotein(a).
And there’s some work going back all the way to Linus Pauling that you can minimize the effects of an elevated lipoprotein(a) by taking Vitamin C, strengthening the wall of your artery, taking some amino acids called Lysine and Proline, and that they may prevent the damage that lipoprotein(a) may do otherwise.
So there is, finally, there actually is a very strange therapy where, much like dialysis, you can get your blood cleansed through a filter. And this is an FDA approved treatment of people like that little girl I mentioned, Stormie Jones, if she were still alive today. That’s a therapy that would be used for somebody with a familial super high cholesterol.
But that filter also takes out lipoprotein(a), so if somebody has a very high level and vascular disease, that’s an option. So, it’s important, I believe, for people to measure their lipoprotein(a). And again it’s genetic, but I mentioned some things you can do.
[Damien Blenkinsopp]: Great, great.
[46:36] So one that I’ve been using for a long time is high sensitive TCRP. Is that something you find useful?
[Joel Kahn]: I do. We’ve been measuring C-reactive protein for decades, because we were measuring it to assess rheumatic fever, so it has a history going back literally decades and decades. But then along came a patented test, the high sensitivity test, and that seems to be more reflective of artery wall inflammation.
And inflamed arteries are more prone to suffer heart attack, stroke, clot and the rest. So you do not want an elevated high sensitivity C-reactive protein. And you want to measure it. And it is highly correlated with increased risk.
So then I’d get on a search for why it might be elevated, and most common would be abdominal obesity, poor nutrition, a lack of exercise, poor sleep or sleep apnea. But you can also look for occult causes like gum disease, periodontal disease and such, unsuspected prostate disease, prostatitis, and probably a diseased gut. Our Western processed foods, high in salt, sugar, and fat causing gut disorders. Lack of adequate microbiome health probably causes inflammation.
So you’ve got to work on the entire patient in a holistic way.
[48:04][Damien Blenkinsopp]: And so I don’t think we’ve really covered this properly, but inflammation is directly related to heart disease as well? Or is it a bit more of a wavy line?
[Joel Kahn]: Yeah no it’s prime time to measure inflammation and high sensitivity C-reactive protein. There’s also a number of other markers out now, like myeloperoxidase, and a test called the plaque test that give insight into inflammation in vessel walls and can be quite useful in a comprehensive assessment.
[Damien Blenkinsopp]: Great, great.
So in terms of some of these indicators, like CRP, the lipoprotein(a) , they’ve got others like alpolic protein, the HDL, the LDL, none of these are binary, as I understand them.
So if someone has a high CRP score, say it’s four or something like that, is that a sure thing that they have some kind of heart disease risk as well? Or could it just be related to some inflammation, or something like that.
You’re really using these as indirect indicators and you can’t trust the picture from that, but it’s just kind of a notice [that] I should go see a physician and investigate maybe if it’s calcium score.
[Joel Kahn]: Yeah. If it’s elevated, it should prompt a search into lifestyle, it should prompt a search into, as I say, gut health, gum health, prostate health, any other. Even though it’s felt to be largely a vascular marker, it’s a marker of the disease and it participates in, actually, vessel damage. But sometimes it can be very frustrating and unclear. I’ve had people with very high C-reative proteins: 40, 50, 60, 70, 80.
There’s a very limited experience with using a shotgun approach, after searching for every possible cause, an antibiotics like minocycline in the tetracycline family. I have been taught that, and I’ve had rare experience to do that with patients after a very thorough evaluation for every other kind of cause of elevated C-reactive protein. And it came down dramatically and stayed down.
[Damien Blenkinsopp]: Great, great.
[50:00] I wanted to tackle one thing. Could you go over the diet you recommend? As background, I’m Paleo and we’ve often talked about ketogenic diets and high-fat diets on here with people like Jimmy Moore and so on.
So could you give your perspective, where you come from with respect to heart disease; what kind of diet and lifestyle are you recommending?
[Joel Kahn]: I like to stay, in every aspect where I can, grounded in the science that’s available. And in terms of artery health, heart disease, survival and heart disease, the weight of the data is not in the ketogenic or Paleo world, the weight of the data like by 100 to 1 in terms of science at least, is in the world of nearly or completely plant based diet.
[Damien Blenkinsopp]: Okay, so is that a vegan diet?
[Joel Kahn]: Yeah. Well vegan, I’ll distinguish those very briefly.
But you can look at epidemiological studies like the Blue Zones, five areas in the world where people live the longest with the greatest freedom from heart disease, none of them are completely vegan. Except actually Loma Linda, California is one of those five Blue Zones, the longest lived community in American, and ten percent of that community is strictly vegan, the other 40 percent are vegetarian, and the remainder are omnivores. They are the longest lived people in the United States and they have the highest percentage of vegans in the United States of any community, because of the Seventh-day Adventist Church there.
So you can look at epidemiological studies like that, or you can look at the data on heart disease reversal, which is a concept that is scientifically sound. Two centers started studying [that], actually three, Nathan Pritikin in what’s called the Pritikin Longevity Center in Florida. He was an engineer, not a physician.
But Dr. Dean Ornish, a cardiologist, began in the early 1980s a lifestyle that is a largely vegan diet. If you really read between the lines its a very low oil, no added oil diet; so less than 10 percent of calories are from fat. He does allow his patients to have some non-dairy fats and some egg whites. So by strict definition it’s vegetarian not vegan.
And he has now pursued that dietary research for more than 30 years. It’s actually approved by Medicare, because the data is so strong that for heart patients it can halt and reverse their symptoms and disease, and minimize their need for medical care.
Dr. Caldwell Esselstyn began the same research project at the Cleveland Clinic in the 1980s, and has similarly shown [with] follow up catheterizations [and] follow up on patients’ health, dramatic reversal of heart disease without stint, without bypass. And his diet is strictly vegan and again under 10 percent of calories are from fats. Kind of the opposite approach to many ketogenic diets.
And, very compelling, Dr. Ornish has taken his program, which is more than diet —- Dr. Ornish emphasizes 30 to 60 minutes of walking, an hour of stress management by meditation or yoga, and group support — and has shown that in prostate cancer you can halt and reverse prostate cancer with his program. And he’s embarking now on a program in breast cancer, which I suspect, but we’ll have to wait, the results will be positive.
So it’s dramatic research, it’s not out of date. I hear some of my colleagues say, “Oh, Dr. Ornish’s data is aged, it’s old.” Well, he’s working with Nobel Prize winning scientists and continuing to put out some of the most cutting edge data on nutrigenomics and epigenetics. And his diet is one that if all of America were to follow to a large part we’d have a tremendous drop in the burden of chronic diseases like dementia, diabetes, cancer and heart disease. Without question; it’s been scientifically proven.
So my recommendation, I lead in Detroit a patient’s support group for people striving to stick to Dr. Ornish, Dr. Esselstyn, the Pritikin program, the Dr. Neal Barnard, you know, reversing diabetes program. And we have about 1000 volunteer people in the area that get together for meetings and group sessions, and it’s been profoundly effective in improving their health at very low costs, very grass roots.
[54:19][Damien Blenkinsopp]: Yeah. So what do you think of the Paleo principles of dairy and grain avoidance? Would you include those in your recommendations, or are those not relevant?
[Joel Kahn]: Sorry, the question was about grains?
[Damien Blenkinsopp]: Yeah, grains and dairy, in general.
[Joel Kahn]: I’d love everybody to stop eating dairy. I don’t view it as a health food in any setting, and it’s a tremendous burden on animals and the environment. And if somebody is not willing to eliminate animal products from their diet but would be willing to eliminate dairy, it’s one of the most frequent food allergens that people react to. It may be involved in the pathogenesis of Type 1 diabetes in children and young adults.
I wish we could legislate a dairy free world. Even the Harvard School of Public Health has advised greatly minimizing your dairy intake and replacing it with healthy hydration, like water, teas, and coffee, unsweetened; even alcoholic drinks, to a limited degree.
But grains, I know it’s contentious. I have had the pleasure of spending time with Dr. Bill Davis of Wheat Belly, Dr. David Perlmutter of Grain Brain, and I think also a name that’s not as well known, Dr. Alessio Fasano, who’s an Italian scientist now at Harvard who’s really doing amazing research on what grains do to Celiac patients and what’s the actual molecular pathways.
And I tend to favor Dr. Fasano, who I think I’m fairly quoting that one percent of the population is showing signs of Celiac disease, six to seven percent of the population if tested shows signs of gluten sensitivity. And that leaves over 90 percent of the population that neither has Celiac nor documented gluten insensitivity and if they’re reacting to grains, they’re reacting very briefly in a way that’s not a big deal.
And they should be part of a healthy diet. If you look at the scientific data, which I just reviewed and published a blog on in the past six weeks, even just in the last two years the data on whole grains and health is an amazingly strong body of data for survival, for freedom from heart disease, freedom from diabetes, freedom from cancer.
And it’s always a question, what’s it substituting? If you’re eating whole wheat pasta, whole wheat bread or wheat germ you’re probably not eating donuts and fried food and vending machine food because you’re exhibiting an intelligence in a selection on the healthier part of the spectrum.
So, I always encourage my patients that are having problems, take a four week elimination diet from gluten. If you’re having runny noses, rashes, if you’re having unexplained headaches, maybe even for an unexplained cholesterol elevation it could be that it’s inflaming your gut, and four weeks would give us some input on how you’d feel and biological markers.
But I eat whole grains consistently and recommend to my patients they do the same if they’re not in that small percentage.
[Damien Blenkinsopp]: Great, thank you for that clarification.
So if someone is on a Paleo diet or ketogenic high-fat diet, is there a test they could take? Would it be the calcium score, would you recommend that they take that if they want to assess if it’s having some impacts?
[Joel Kahn]: Yeah, well my comment and advice for those that are following a ketogenic diet is if you’re doing it for 10 days to fit into a tuxedo for a wedding, it probably will work and you’re probably not going to do yourself any harm. Long term, again I have to go to science, which there were at least two or three major studies saying long term low-carb ketogenic diets are associated with increased risk of death.
These are studies involving tens, and tens, and tens of thousands of people; yes, they’re databases, yes they’re association studies, but they are strong because there is no data that you live longer with a ketogenic diet. And in the last nine months there’s been specifically a study that ketogenic diets after heart attack are associated with the increased risk of dying.
So I strongly advise my patients not to follow ketogenic diets, and if they choose to, yes I think they should have all the biomarkers. If they don’t know of atherosclerosis then they should be having calcium scoring and possibly the carotid ultrasound testing. But I would advise them against it.
I know it’s all the rage, but it is a stress on the body, it’s a stress on the adrenals. And the healthy carbs found in vegetables, even starchy vegetables and whole grains, are adrenal pleasing sources of nutrition.
[Damien Blenkinsopp]: Great, great. Thanks for the clarification.
[59:00] Winding up, this is kind of a thing that affected a lot of my friends in their 20s. People were working very hard and were taking a lot of caffeine and generally very stressed, [and] we were getting a lot of pains around the heart area.
One of my friends went to a doctor and he said it was just stress and caffeine. I don’t know if you’ve come across this before; is this an issue, or is it just a symptom which isn’t really that important? Maybe too much caffeine or something.
[Joel Kahn]: Yeah. Caffeine in general, I mean it’s interesting. There is some genetic variation, and there is even a blood test you can get that’s a SNP, single nucleotide polymorphism, it tells you if you metabolize caffeine rapidly or slowly. If you metabolize it slowly, it’s going to hang around longer and give you more tendency to feel jittery or racing heart. And if you metabolize it rapidly, otherwise.
But with that aside, if it doesn’t bother you, caffeine is, in most studies, a health food. Now of course, like everything, you dump in some manufactured whitener and sugars, and you don’t have coffee anymore you have some modified, processed, anti-health drink. And certainly a frappuccino isn’t a cup of coffee.
But black coffee, dark roasted coffee two or three cups a day is generally a good boost in the morning, a good brain support. I always would cut it off about two in the afternoon so it doesn’t interfere with sleep. It’s a rich source of antioxidants.
There’s a little concern that your readers may know about that some coffees may be contaminated with mycotoxins, fungal toxins. You don’t really know it because it’s not measured and reported on American coffee sources; it is in Europe, and in fact there’s limits in Europe where they can’t be sold. Coffee beans sit outside and they can get moldy, and the mold can get into the coffee beans.
So you can ask around where you buy your coffee; it’s not a topic that a lot of people know about, and it may be a source of some illness for some people that are sensitive or are drinking lower quality coffees that may have mycotoxins.
With those couple of comments aside, I am pro-coffee. My heart patients ask me, I tell them enjoy a cup of black coffee. I certainly also urge them to enjoy green tea, or any of the teas actually; herbal teas, hibiscus tea, chamomile tea before bed [is a] wonderful source of soothing and sleep support.
[Damien Blenkinsopp]: Right. So it doesn’t sound like there’s any specific mechanism there which would be giving people heart pain from just coffee. Maybe something more like stress?
[Joel Kahn]: Right. There should be no heart pain.
[Damien Blenkinsopp]: Okay, great.
[1:01:32] So, where should someone look first to learn more about your topic? Are there any good books, your books, or presentations on some of the subjects you referenced?
[Joel Kahn]: Sure. I [1:01:41 unclear] appreciated that, and I probably do need to get back to some hospital rounds here. But I do have an active website at www.drjoelkahn.com. And all the blogs and TV interviews and podcasts and things I’ve done over the last few years are there. I encourage anybody to take a peek.
I do have two books out. Last year The Whole Heart Solution, published by Reader’s Digest. And this year a self-published book — but they’re both on Amazon — it’s got the title, Dead Execs Don’t Get Bonuses: How to Survive Your Career With a Healthy Heart, which I think is an important topic and the title has caught a lot of people’s attentions. It’s a real plea to not be one of those dead execs, or dead anybodys, for as long as you can.
I would encourage anybody to read anything by Dr. Dean Ornish, Dr. Caldwell Esselstyn, Dr. Neal Barnard, Dr. Garth Davis in Houston. All active scientists, researchers, clinicians that I think are speaking from the heart about overall health and sort of bucking the trend that all fats are good and animal products are benign.
We just don’t speak about the environment enough. We just don’t speak about animal rights enough, and we have to have a holistic approach to our plate; our plate represents an impact on forests and impact on our waterways and impact on our grandchildren’s world. And our plates represent a process that is very often extremely cruel, extremely unfair to beings that feel and sense pain and terror. And it’s as if we can’t talk about that.
We have labels — Paleo, Mediterranean, Ketogenic — but that’s only partial descriptions. I like to eat a kind diet and my plate is filled with kindness. So I hope that spills into my life as much as possible.
[Damien Blenkinsopp]: Thanks so much for all of those references. That’s a lot of material for people to get through. We’ll put all this stuff up on the show notes, of course.
[1:03:50] One last question. In your own personal life, are there biomarkers that you track on a routine basis? What do you do in terms of collecting data for yourself, for optimizing health and performance, or whatever?
[Joel Kahn]: Yes. I mean, I’ll do inflammatory markers like C-reactive protein, advanced lipid tests like LDL particle number and size. I’ll look at my Vitamin D levels. I’ll look at my male sex hormone, estradiol, total and free testosterone; I try and keep those optimal through natural ways, exercise, weight loss, weight lifting and such, healthy diets, toxin free diets that don’t interfere with the process. Blood sugar and insulin sensitivity, fasting glucose, hemoglobin A1C, important markers. So those would round out the majority that I’m doing: homocysteine level
[Damien Blenkinsopp]: Great, thank you very much for that.
Well Joel, it’s been really great to have you on the show. You know, we’ve covered a lot of ground today and a lot of markers, and I’m sure it’s going to clarify a lot for the audience.
[Joel Kahn]: Well there’s so much people can do. They’re in control of their health. And it starts with realizing that, and realizing the power of food, the power of fitness, the power of abstaining from smoking, the power of sleep, the power of friendship, and then getting credible information. And your podcast has done a wonderful job [with that], and I’m very honored to be able to share with your audience.
[Damien Blenkinsopp]: Thank you.
[Joel Kahn]: Have a great day, sir.
[Damien Blenkinsopp]: You too.