There is growing evidence that ketone bodies, whether they come from fasting, keto diets, MCTs or exogenous ketones have potential applications across many areas from longevity to performance, to health and mitigating some of the risks and symptoms of certain diseases like cancer and neurologically inclined deceases. As such the whole ketone body area is what I call a high leverage area due to the many potential upsides.
So I’ve personally been investing more time into experimenting in this area as the payoff for that effort, looks pretty promising. You’ll have noticed that I’ve done a fair amount of fasting and since late 2015, that also includes the exogenous ketones and playing around with the ketogenic diet. More to come on my results with all of those in future episodes.
This interview is a very in depth look at many of the applications of ketone bodies and the nuances of their use in the body.
– Dominic D’Agostino
Today’s guest is Dominic D’Agostino. Dominic has something that I found relatively rare but makes for extremely valuable interviews. He has a combined prospective coming from both research and self-experimentation. He has a considerable amount of lab work and research specifically done into ketogenic diets, ketones, ketone driving supplements and a growing number of applications. And he has done a lot of his own self-experimentation for many years in this area.
Dominic is currently an associate professor in the Department of Molecular Pharmacology and Physiology at the University of South Florida, and he’s also a senior research scientist at the Institute for Human & Machine Cognition (IHMC). His research is focused on developing and testing ketogenic diets, ketone supplements, and amino acid formulations for a broad range of therapeutic and performance applications.
His laboratory uses in-vivo and in-vitro techniques to understand the physiological, cellular, and molecular mechanism of nutritional ketosis and supplement formulas. His current efforts are focused on evaluating different methods for inducing and sustaining nutritional ketosis and how this can be optimized to the specific individual and applications. So, we’ll see in today’s interview that there are a lot of nuances and it’s a bit more complex than just boosting your ketones.
Dominic’s research is supported by the Office of Naval Research, The Department of Defense, Support Supplement Companies, and Private Foundations.
Special Note: In the interest of full disclosure, since late 2015 I own a company (Ketosource.co.uk) that develops ketogenic and ketone driving supplements, foods and drinks for the UK.
The episode highlights, biomarkers, and links to the apps, devices and labs and everything else mentioned are below. Enjoy the show and let me know if you want more on this topic in the comments!
What You’ll Learn
- Using exogenous ketones to mitigate some of the impairments of sleep deprivation (all nighters, or jetlag) (5:50).
- How the stress response from scenarios like jetlag will kick you out of ketosis (and can be compensated for via exogenous ketones) (13:00).
- Dominic’s background research and how his career has evolved to working on ketone bodies and ketogenic diets and their applications (14:50).
- Recent research with mice that may indicate that ketosis reduces anxiety (17:00).
- Screening a range of different naturally derived exogenous ketone agents for their therapeutic and performance benefits (18:40).
- A once to twice per year fast or nutritional ketosis protocol for potentially activating a range of beneficial genes (37:50).
- The press-pulse ketone body strategy for the management of cancer (40:40).
- The benefits of the ketogenic diet for the management of epilepsy over the pharmaceutical alternatives (49:20).
- Using the ketogenic diet to restore normal appetite regulation (50:15).
- The various health, performance and longevity applications for ketone bodies (52:00).
- Potentially reducing tremors in Parkinsons and Alzheimers with the use of ketone bodies (57:10).
- Evaluating the legitimacy of recently raised safety and effectiveness concerns related to ketone salts and MCTs based on scientific facts and their track record over the last two decades (1:01:10).
- How racemic exogenous ketones suppress glucose more effectively than non-racemic exogenous ketones (1:13:40).
- Using MCT oil powder as a staple product for coffee, baking and protein shakes to boost the ketogenic profile of your diet (1:16:00).
- Avoiding liquid meals in order to be able to elevate protein intake higher while remaining in ketosis (1:18:00).
- What a typical ketogenic day looks like for Dominic in terms of blood ketone measurements from morning to evening and how he optimizes it (1:20:00).
- How Dominic has identified his optimum ketone and Glucose-Ketone Index ranges for mental performance (1:21:00).
- To standardize and control for your blood ketones and glucose you need to be fairly sedentary (1:34:10)
- Dominic D’Agostino’s recommended self-experiment with the largest potential upside with the tactic to test and biomarkers to track (1:42:00).
Thank Dominic D’Agostino on Twitter for this interview.
Click Here to show him some appreciation for doing this interview!
Dominic D’Agostino
- KetoNutrition.org: Dominic D’Agostino’s home site where he has links to many of his research interests and other resources for ketogenic diets and ketones.
- University of Southern Florida Bio page: Includes a list of Dominic’s research papers.
- Metabolic Optimization Podcast: A new podcast where Dominic and Travis Christofferson discuss different aspects of metabolism including ketone bodies with guests scientists. Dom mentioned the Bruce ames interview, Thomas Seyfried interview and Dr. Adrienne Scheck interview.
- Dominic’s Meta.Science Page: A list of all his published research papers and concepts.
- Social Media: Dominic’s Twitter and Facebook
- Metabolic Therapeutics Conference: The biggest conference covering the ketone topic. The conference brings together Dominic, his colleagues, and many other researchers in the metabolic therapy and ketone space. The next conference will be in late Jan/ early Feb 2017.
- IHMC (Institute for Human & Machine Cognition): Dominic also works with and recommends some of the work and podcasts in this research organization.
Recommended Self-Experiment
- Tool/ Tactic: Start Intermittent Fasting with fasting windows of 18 hours and eating windows of 6 hours each day. Dom recommends listening to Matt Mattson’s talk on IF before you start.
- Tracking: Get some baseline lab tests before you start the IF and again 3-4, and/or 6-8 weeks afterwards to see the positive impacts. Your lab tests should include fasting glucose, triglycerides and hs-CRP.
Tools & Tactics
Diet & Nutrition
- Well Formulated Ketogenic Diet: The high fat, low carb, moderate protein diet that puts you into ketosis with typical blood ketones of between 0.5 and 3 mmol/L depending on execution and the person. Not suggested for children, teens or people in their 20s with good insulin sensitivity in general.
Foods Dominic Makes Particular Use of:- Coconut Cream: Combines the fats with some of the fiber from the coconut flesh. Coconut cream is also known as Coconut Butter.
- Ghee (Clarified Butter): Butter that has had the dairy proteins removed to leave solely the fats. As such it is considered dairy-free.
- Wild Sardines
- Sour Cream with Live Cultures: Didn’t find a link to this – if you know a good source please let me know in the comments.
- Intermittent Fasting: Sometimes referred to as short-term fasting due to the typical 16 hour to 20 hour fasting window. Dom noted that he has spoken to a fair number of high-performing CEOs doing this routinely recently.
- Fat Fast: A modified intermittent fasting protocol whereby you restrict caloric intake in the fasting window (e.g. 18 hours of day) to some fats, exogenous ketones and/ or MCTs instead of a pure fast (no food or calories). Dom finds this method effective and that he tends to be less hungry going into the eating window (i.e. 6 hour window).
- Periodic Fasting: Typically refers to fasts spread out by once per week or once per month. We’ve done past self-experiments on the once per month periodic fasting protocols via a 5 day fast, 10 day fast and fast-mimicking diet.
Fasting Protocols
Supplementation & Drugs
Exogenous Ketones
Dominic’s lab has looked at a variety of exogenous ketone formulations in different scenarios and applications. Amongst their papers are included improved blood lipid profiles1 and non-toxic metabolic management of cancer2.
MCTs and C8 (Caprylic Acid)
- Brain Octane: Pure Caprylic Acid (C8) from Bulletproof Nutrition.
- Keto8: Pure Caprylic Acid (C8) oil from KetoSports.
- Quest MCT Powder: MCT powder that Dom is using as one of his staples mixed into coffee for example.
Dominic’s Sleep Deprivation Effects Mitigation Cocktail
- Exogenous ketone: Take your pick from one of the exo ketones listed above. Is beneficial to combine with MCTs such as C8 or MCT powder.
- Caffeine: Needs no introduction – use coffee or your other favorite
- Huperzine A: A nootropic herb used for cognitive enhancement via modification of acetylcholine levels.
Drugs
- Metformin: A drug which is used to improve blood sugar regulation in diabetes. Researchers are looking at its wider applications with cancer treatment as it has been found to inhibit insulin secretion.
- Ringer’s Lactate: The long term use of this racemic solution was noted as evidence as to the safety of racemic ketone salts.
Tech & Devices
- Hyperbaric Oxygen Therapy: Increasing the amount of oxygen in the body with the use of a hyperbaric oxygen tank which uses air that is more highly saturated with oxygen and which is compressed. Dominic has worked on research with Doctor Thomas Seyfried looking at its application for cancer therapy in combination with ketogenic diets3.
Tracking
Biomarkers
- Glucose: Dom suggests aiming to keep values between 60 and 80mg/dl and that if you can maintain this all other biomarkers should be fine.
- Glucose Tolerance (OGTT): The Oral Glucose Tolerance Test is a glucose challenge test whereby you take a certain number of grams (e.g. the typical standard is 75 or 100 grams) of glucose and test your body’s ability to regulate glucose and bring your blood glucose back into normal range over a certain time period (e.g. 2 or 4 hours). Dom used the OGTT to assess his insulin sensitivity – the more insulin sensitive you are the quicker your blood glucose returns to normal fasting levels e.g. between 60 and 80mg/dl optimally.
- HOMA (Homeostatic Model Assessment): An alternative method to the OGTT used to assess insulin sensitivity/ insulin resistance.
- Glucose-Ketone Index (GKI): This index was conceived by Thomas Seyfried and discussed in detail with him in episode 16. It assesses the weighting of the metabolism towards ketone vs. glucose. Lower values are ketone driven metabolisms and higher value (especially over 20) can be associated with heavy glucose metabolisms associated with chronic disease. Dom brought a new angle to this marker with an optimum everyday target he shoots for of between 2 to 4. Previously we discussed Thomas Seyfried’s recommendation of undertaking a 5 to 7 day therapeutic water fast once or more times per year targeting a GKI value under 1.
- Triglycerides: Dom believes this is the most important biomarker to watch. Optimum levels estimated as below 40mg/dl.
- HDL: Higher HDL levels are said to be protective and beneficial. Dom’s value are around 90 mg/dl.
- LDL: Dom believes keeping values in the normal to normal high reference range are perhaps optimal. This puts levels at approx. 80mg/dl to 110mg/dl. We previously discussed LDL in more depth in episode 7.
- hs-CRP (high sensitivity CRP): CRP (C-Reactive Protein) is a very common marker of inflammation that is used to assess cardiovascular risk amongst other things. It tends to drop on a ketogenic diet. Dom’s values have been between 0.1 and 0.2 since he quit dairy (Note: Damien’s levels are also at this level).
- IGF-1: IGF-1 was discussed in more detail in our FMD episode. Dom’s IGF-1 values dropped significantly after quitting dairy.
- Heart Rate: Typically heart rate is measured as the biomarker Resting Heart Rate (RHR) for standardization, which is an average of the beats per minute. See episode 1 to understand the use of RHR.
- Blood Pressure: Optimum ranges are for systolic between 90 and 120 and dystolic 60 to 80 expressed as for example 110/70 mm Hg.
Glucose/ Ketone Metabolism
Lipids
Other
Lab Tests, Devices and Apps
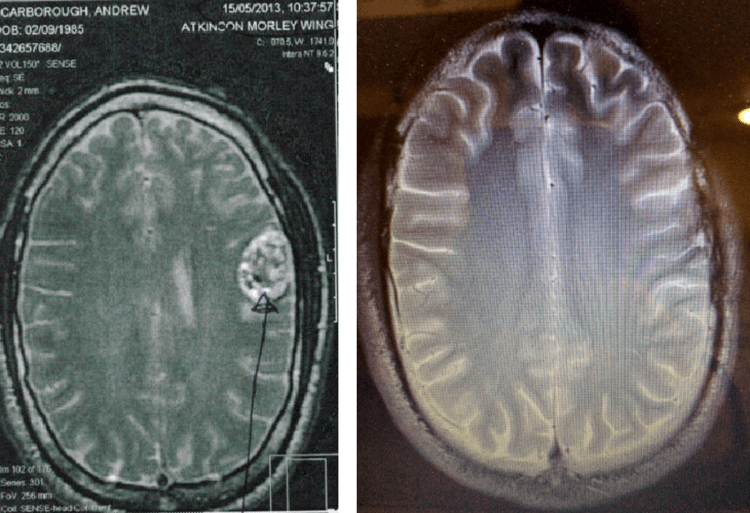
- Fludeoxyglucose PET (Positron Emission Tomography): This scan was discussed in depth in a previous episode with Gene Fine on quantifying cancer. Fludeoxyglucose is the radioactive pharmaceutical used with PET to track glucose density in the body.
- Fit Bit Charge: Dom uses this for tracking sleep quality primarily.
Devices for Measuring Glucose & Ketones
The different approaches to measuring ketones provide different perspectives on your ketone metabolism. These can be looked at in terms of the ‘window of snapshot’ that they represent. Some methods have a snapshot of a longer duration, so provide more of an average reading, while others provide a direct status of that exact moment.
Moving from the more average-based value end of the scale to the more direct status end you have:
- Measuring ketones via the urine (via the ketone body acetoacetate) has the longest snapshot with it representing your ketone values over the last 5 to 6 hours.
- Measuring via the breath (the ketone body acetone) has a smaller snapshot window of the 2 hours leading up to the measurement.
- Measuring via the blood (via the ketone body beta hydroxybutyrate) provides you a snapshot of your ketone level at that exact moment.
The various devices available for glucose/ ketones testing and mentioend include:
- Urine Ketone Strips: . Both hydration status and becoming keto-adapted interfere with the measurement values provided by this. Dominic recommends starting with urine test strips as they are the cheapest and effective until you get keto adapted.
- Ketonix Breath Meter: Currently the only breath acetone meter. If you are moderate to high on this meter you are effectively in ketosis (i.e. typically over 0.5 mmol/L). Dom recommends this in particular for epilepsy since breath acetone has been correlated with seizure control.
- Precision Xtra: The most popular meter for testing blood glucose and ketones in the U.S. Has a broader reference range than the NOVA providing values for lower blood glucose levels instead of the LOW error.
- Freestyle Optium Neo: Freestyle Optium Neo is the upcoming replacement for the PrecisionXtra, it comes from the same company and has similar functionality – the only difference in the meters seems to be a rebranding exercise.
- Novamax Plus: Novamax Plus is a slightly cheaper meter with some greater accuracy and sensitivity concerns than the Precision Xtra or Freestyle Optium Neo.
- Dexcom G5 CGM: A Continuous Glucose Monitor that Dom is about to start experimenting with for blood glucose optimization. Peter Attia has also been using this tracking device recently to optimize blood glucose regulation. We discussed continuous glucose monitoring and the devices available in episode 43
Blood Glucose & Ketone Monitoring Systems
Other People, Books & Resources
Books
- Ketogenic Diets: Treatments for Epilepsy and Other Disorders: By John M. Freeman – One of first books Dominic read providing a good overview of the Ketogenic Diet.
- Tripping Over the Truth: The Metabolic Theory of Cancer: Covers the history of the work on the metabolic theory of cancer – written by Travis Christofferson.
- The Art and Science of Low Carbohydrate Performance
People
Researchers
- John M. Freeman: Of Johns Hopkins university, known for bringing ketogenic diets back into use for treating epilepsy.
- Dr. Thomas Seyfried: One of Dominic’s close colleagues in research who spoke to us on fasting in episode 16.
- Dr. Adrienne Scheck: Research with the ketogenic diet including moving it into clinical trials.
- Dr. Eric Kossoff: A neurologist at johns hopkins and one of the pioneers of the use of the ketogenic diet to treat epilepsy.
- Mark Mattson: Broadly known for his work with fasting, and particularly his TEDx Talk on fasting. Dominic specifically recommended this podcast interview Matt did at IHMC on intermittent fasting.
- Eugene Fine: Eugene’s work using PET scan was discussed by Dom, and we also spoke to Eugene about this work in episode 36.
- Dr. Richard Veech: Dr. Veech is renowned for his work on ketone metabolism and the benefits of ketone bodies, including an often cited review paper4. He appeared recently on two podcasts (Ben Greenfield, Bulletproof Exec) where he discussed his concerns over the use of ketone salts and MCTs in terms of safety and effectiveness. Dom addressed his concerns in this interview.
- Susan Masino
- David Diamond
- David Ludwig
- Adam Hartman
- Colin Champ
- Jeff Volek
- Dr. John Roe
Other Mentions
- Tim Ferriss: Has been experimenting with the breathe hold extending effects of ketone bodies via ketogenic diet and exogenous ketones.
- Ben Greenfield: Has been experimenting with using exogenous ketones for free-diving.
Organizations & Companies
- Companies developing Ketone products: Ketosports, Ketosports, Prüvit, Kegenix, Forever Green and Quest Nutrition.
- Scivation: Company with Dom’s recommended BCAA supplements.
Other
- Ketogenic Diet Resource: Site authored by Ellen Davis that is a good “go-to-resource” for everything keto.
Full Interview Transcript
[Dominic D’Agostino]: Thanks for having me, Damien.
[Damien Blenkinsopp]: Yes, it’s great to connect. So you’re just back from a trip to Budapest and you just told me that you’re doing something to bypass the jet lag?
(05:42) [Dominic D’Agostino]: Yeah. Sometimes depending on circumstances I try to prioritize sleep and try to get between six to seven hours sometimes eight on the weekends if I can. But in the absence of sleep, I like to test certain things.
Usually happens once every month or two or I’m going to have to skip one night completely and have to get thrown right back into the fire of work again. I’m doing that now, and testing some different exogenous ketones in combination with caffeine and some Huperzine, and a few other little things in a stack formula that I’m working on.
It seems to be working because I’m functioning and I’ve been able to manage my tasks in a way that allows me to get stuff done.
[Damien Blenkinsopp]: So, this could be a new jet lag formula? Or if you want to keep going on sleep deprivation and work for a night or something…
[Dominic D’Agostino]: Yeah. So, inevitably people will come to the situation where they have to meet a deadline and stay up all night to get something. I don’t recommend doing it all the time because you can get burned out. There is no pill that you can take that will substitute for sleep.
But there are ways to extend your productivity and performance with two or three days of no sleep. I don’t like when those situations arise, but I worked on ways to mitigate some of the impairments that accompany that.
(07:13) [Damien Blenkinsopp]: That’s excellent, that sounds like another application for exogenous ketones I had not thought of. I know there are a whole bunch I want to discuss with you because it seems like there’s quite a few of them. So now if you want to work all night, they can help with that.
I’m tempted actually, what is the mechanism behind that specifically for sleep, is it just a pure energy thing or?
[Dominic D’Agostino]: As far as sleep? Mitigating sleep?
[Damien Blenkinsopp]: Why would exogenous ketones help with?
[Dominic D’Agostino]: Yeah, I think there are several ways that they can help. You can formulate things to provide energy to the brain. There’s various, what we call tricarboxylic acid cycle intermediates, including alpha-Ketoglutarate, creatine – is actually something that could be beneficial to the brain when energy reserves are low, and ketones have a unique effect of being anaplerotic. So if something is anaplerotic it helps to generate the bioenergetic intermediates which include the Krebs cycle or also called the TCA cycle intermediates.
Essentially just helping to energize the brain when fuel flow is low. Many of the TCA cycle intermediates are also precursors to neurotransmitters. For example, alpha-Ketoglutarate is a precursor to glutamate, and then from glutamate through glutamic acid decarboxylase we make GABA.
So, ensuring that we have efficient energy flow to the brain and sort of stimulating anaplerotic reactions and bioenergetic reactions we can replenish the neurotransmitters. Being in a state of ketosis too, can also be glycogen sparing.
I always had the opinion that when we sleep, part of the function of sleep not only restore neurotransmitters but to also restore brain glycogen levels.
Glycogen is actually stored in the astrocytes of the brain. Astrocytes are not just for support cells they have a really important function that pertains to glutamate recycling and sort of dynamic interactions with the synapses and recycling of neurotransmitters and restoring brain glycogen levels is a function when we sleep.
I think we need to look into this more but I have a theory that being in a state of strong ketosis could prevent some of the glycogen depletion that accompanies a normal day in a person that is normally sort of carbohydrate fed.
Where the brain is sucking massive amounts of glucose but if you’re ensuring that it gets a steady fuel flow of ketones it’s going to be glycogen sparing in that way. Sort of like what Jeff Volek is doing with the athletes and it showed in a recent metabolism paper, that being keto-fat adapted and keto-adapted can actually be very glycogen sparing. If you look at the muscles of lead athletes on a carbohydrate restriction, amazingly their glycogen stores are topped off in the muscles.
I think the same thing is happening, I see no reason why it wouldn’t happen in the brain. Our energy reserves in our brain tank, adenosine goes up, neurotransmitters are depleted – we want to sleep. Being in a state of ketosis can slow that process, and exogenous ketones can be a tool in a toolbox to help with that.
[Damien Blenkinsopp]: That’s really fascinating. It’s like the biochemistry of sleep, we’re getting tired and I think we understand on a very basic level but you’ve just broken down quite a few mechanisms which lead to us needing to sleep and how to counter them.
[Dominic D’Agostino]: Yeah, sleep is a really complicated subject. I did my Ph.D. in a pulmonary critical care department that was also a sleep lab. So I sat in on a lot of rounds and meetings with residents and fellows about the mechanics of sleep.
It’s just a fascinating subject, and something I’ll probably get more into research wise. But I do teach the medical students about obstructive sleep apnea and central sleep apnea, that’s some of the research that I did in my Ph.D.
(11:22) [Damien Blenkinsopp]: Excellent, and you’re on a keto-diet as well right still?
[Dominic D’Agostino]: Yeah. I maintain that but I also like to cycle a little bit because I think a lot of the therapeutic and performance enhancing benefits can be achieved with nutritional ketosis but I also think it’s good to have relative changes.
Not to stay on something all the time, but to adjust your macronutrients a little bit, and also maybe your calories a little bit, and occasionally fasting. These relative changes can produce some pretty good performance and therapeutic effects.
[Damien Blenkinsopp]: It’s kind of like exercise like promoting metabolic flexibility, is that where you’re coming from?
[Dominic D’Agostino]: Yeah, that was what I was going to say and relate it back to a hormetic effect where relative changes are good. For a while, I just stayed on the exact same ketogenic diet for a long time and I started adjusting and playing around with different supplements and I realized it’s good to sort of adjust the diet and even adjust your calorie levels sometimes. My life is variable, it kind of fits on with my lifestyle too.
[Damien Blenkinsopp]: I feel the same way. I’m probably doing the something a bit more varied these days. So, it’s just interesting, you said you are basically stacking exogenous ketones for sleep on top of your keto diet. Does that push your levels quite high?
[Dominic D’Agostino]: At least doubles or maybe triples where I would be. I have noticed in the past that if I just stick to my normal diet and I cross time zones. I’ve been in at least a dozen time zones for the last month and a half, two months.
When I do that and I miss a complete night of sleep, coming from Southeast Asia completely flips circadian. I realized that I get a stress response from that I think my cortisol goes up, my sympathetic nervous system can be activated. And I notice that can kick me out of ketosis a little bit or I’ll have levels that are — I would predict there would be much higher based on the macronutrient profile that I’m eating and even fasting.
So, I find that exogenous ketones can sort of help in those situations where I put my body into an unaccustomed stress.
(13:36) [Damien Blenkinsopp]: That’s very interesting. I’ve started to use some of the supplements, exogenous ketones for different scenarios a bit like that situation but we can talk about that later. So, I wanted to give people a background, would you say your focus area is ketones, ketogenic diet? Is that what you’d call your focus area of research?
[Dominic D’Agostino]: Yeah. I’m classically sort of trained as a neuroscientist. I did my PhD in something very specific, it’s patch clamp electrophysiology where you measure from individual neurons and you record the membrane potential, firing frequency input resistance of individual neurons, either in cell culture or in a brain slice, and studying pharmacology and the metabolic activity. I became very interested in observing fundamental neuronal activity.
I became very interested in the metabolism that was supporting that. I realized that the life that I was seeing on the amplifier of the oscilloscope, these neurons firing was completely a result of the electrochemical and the electrical gradients between the neurons, they’re like little batteries.
That was generated completely by the metabolic activity so cells they need to maintain negative 56 kilojoules per mole of energy and they will do anything to do that. Some substrates and some means of generating ATP are more efficient than others. In my early work, I was actually looking at lactate.
I was interested in Ringer’s lactate, so racemic Ringer’s lactate is actually used on the battlefield and also in surgery when people have a lot of massive blood loss. Lactate is extremely efficient fuel, and I studied hypoxia in the brain and ischemia, and I was interested in lactate for that. That got me interested in this whole idea of developing and testing metabolic substrates to preserve and enhance brain energy metabolism in the face of extreme environments.
Our work for the last decade has been funded by the military. So I’m interested in particular situations that would accompany military operations, like a navy seal using a closed circuit rebreather with high levels of oxygen. He’s susceptible to a limitation of his mission, would be oxygen toxicity seizures so the fundamental neuroscience that I learned in my Ph.D.
I applied that to developing and testing metabolic base therapies to preserve that cognitive function and metabolic resilience in the environmental extreme of high-pressure oxygen. That’s sort of a fun thing to do because there’s many ways to do it. I’m always looking for the next, or the optimal formula, of ketones and that’s why we don’t focus on any one particular exogenous ketones. We screen a variety of ketogenic agents or formulas of them to identify the one that’s most neuroprotective or anticonvulsant.
Now, we do cancer studies and we do wound healing, performance applications – and it might be a different ketone for different applications and we’re testing that now. In Budapest, we actually presented some really interesting work on anxiety. So if we induce a state of nutritional ketosis, the anxiety levels go down pretty significantly. In a rodent model, they’ll spend more time in like an open-arm of an elevated plus maze.
Perhaps that reduced anxiety can play a role in reducing seizures too, so it’s another variable that we need to look at. I probably went off on a tangent. My background was neuroscience and now I do what I would call a nutritional neuroscience or metabolic based sort of strategies to target neuronal processes and neuroprotection.
(17:43) [Damien Blenkinsopp]: How many years have you been doing this now?
[Dominic D’Agostino]: I started neuroscience research as an undergraduate in 1997. So, it’s going on about — 1996 or 1997 — so about 20 years now I’ve been into neuroscience research. The office of navy research, post-doctoral fellowship, was the first large grant money that I’ve got, and that was 10 years ago.
It took me about four years to recognize that the most potent strategy for oxygen toxicity for mitigating that, which I was being funded to do would be a ketogenic approach. Then the ketogenic diet at that time was recognized as something very obscure even just six years ago. So the funding agency really wanted a ketogenic diet in a pill per se.
In addition, to our ketogenic diet research which I feel is also very important we have developed these synthetic and actually naturally derived ketogenic agents to mimic the effects of fasting, the ketogenic diet, and also to further augment the therapeutic efficacy of the ketogenic diet. If the ketogenic diet can only get you to one to two millimolar, and we boost it in another one or two millimolar with exogenous ketones. We’ve realized that, that can be very beneficial.
Not everyone can follow a ketogenic diet including performance applications or for therapeutic purposes.
[Damien Blenkinsopp]: People find it quite hard. I don’t think it’s relatively complex to get into it. I speak to a lot of people who think they’re in ketosis but they’re not.
[Dominic D’Agostino]: Yeah, I do too.
(19:25) [Damien Blenkinsopp]: It’s a little bit tricky I think. So, alas comes the supplementation and so on which could make it easier. I think what’s really awesome about you, you self-experiment as well in addition to your research.
You’re always looking for this stuff and I know you’ve been on a keto diet for a long time, when did you start that?
[Dominic D’Agostino]: Yeah, that’s the fun part of this research that I’m really excited about. Well looking back, I did low-carb diets for a while because I was always into powerlifting, fitness, and nutrition. So, I would experiment, and I was under the impression that being on ketosis was bad.
When I did a low-carb diet or what I call the ketogenic diet, I remember smelling like ammonia. Because it was basically a very high protein, zero carb diet, with a normal amount of fat. Then I got educated I guess, being connected with the folks at John’s Hopkins who are using this on a clinical setting. I read the book by John Freeman and Eric Kossoff at John’s Hopkins, which is a great book, ‘The Ketogenic Diet’ for epilepsy and other disorders that’s out there.
There are one or more popular books on Amazon. I realized wow I didn’t know what a ketogenic diet was. I didn’t realize it has this fascinating history. You know written with Travis Christofferson, we wrote a three part of series on Robb Wolf’s blog about the ketogenic diet the history. When I actually got into the 4:1 ratio ketogenic diet, the John’s Hopkins which is like 90% fat.
And I transitioned into a state of nutritional ketosis, it was kind of difficult in the beginning. After about two or three weeks I adapted quite well and started realizing the neurological benefits. The appetite suppression was pretty extreme it was difficult for me to maintain my weight even.
(21:16) [Damien Blenkinsopp]: In terms of losing weight?
[Dominic D’Agostino]: Yeah, because my protein level was really high. I think I was getting probably 300 grams of protein a day which is really high. So, I had to drop that down to about 100 grams of protein a day to hit those macronutrient ratios.
Probably about 120 grams a day of protein, which was a relative change that was really low. When I reduced my protein to 1/3 but elevated my fat, and I still kept going to the gym. But at the time my academic career was sort of going full steam and I was in the gym less, but still making it once or twice a week.
My weights that I was handling on major exercises were maintained so I realized that being in a state of nutritional ketosis had a pretty profound anti-catabolic effect. So, I figured I’d be wasting away if I wasn’t getting my body all these protein. But I was amazed that I could eat.
I even started experimenting and went down to like 60 or 80 grams of protein a day. Even after a couple weeks and months I was able to still move the same weights.
So it really blew my mind that shifting the metabolic physiology to being more fat and keto-adapted had this sort of protein sparing anti-catabolic effect. Which makes sense if you look at it through like an evolutionary lens.
So if we stop eating and we didn’t make ketones to fuel this big, highly energetic organ in our head. If the ketones weren’t providing fuel for our brain we would liberate a lot of gluconeogenic amino acids from the skeletal muscle, and we would quickly waste away probably in a week or two, for a lean individual. That’s important to recognize in the context of using a ketogenic diet for a weight loss strategy and also for body composition.
For example, athletes that need to make weight which many sports do — wrestling, boxing, mixed martial arts – keeping that power to weight ratio is important. We think from the studies that we’ve done, we actually just got a study approved finally for publication yesterday showing elite level athletes or advanced lifters that the ketogenic diet is quite effective for body composition alterations and preserving strength and muscle strength and performance.
So that should be out pretty soon in general strength and conditioning. We realize that the ketogenic diet has far more applications than just pediatric epilepsy, which was it’s original application. We’ve probably studied about 10 different applications now in our lab.
(23:59) [Damien Blenkinsopp]: Excellent. So I wanted to run through some of those applications. First of all taking a step back because you mentioned lactate earlier. I think the majority of us assumes that glucose is the main metabolism. Then we learned about ketones and we think maybe there’re two substrates that we’re using for metabolism.
As I understand it, it’s a lot more complicated right? That we’re using a number of different fuels at any time?
[Dominic D’Agostino]: Yeah. I think the big ones for brain metabolism, which our laboratory originally focused on and now we’ve branched off, would be glucose would be the primary fuel for most people. Then ketones are sort of a backup fuel.
If you’re on a ketogenic diet, you’re running this hybrid engine and you’re using both fuels at the same time. With ketones probably the most efficient of the two. Then lactate too.
When we exercise, we mobilize a lot of lactate and put a lot of lactate back into the bloodstream through what’s called the Cori cycle. We convert that back to glucose and then replenish liver glycogen or muscle glycogen. But that lactate can also go past the blood brain barrier across which is called the monocarboxylic acid transporters and provide a source of energy for our brains.
Lactate metabolism in the brain can also occur under conditions of oxygen deprivation, so it may be beneficial. That was also an interest in my earlier work, using lactate to preserve bioenergetic processes in the absence of oxygen. What we call hypoxia or anoxia, which is a complete lack of oxygen.
Interestingly ketones can generate more ATP per oxygen molecule consumed. In a hypoxic situation, ketone metabolism may also be able to preserve the bioenergetic state of the brain. That’s something that we’re also looking into hypoxia and ischemia protection of the brain with various fuels, ketones, lactate preventing or an alternative substrate to glucose.
In certain situations, neuropathologies and even a hypoxia, stroke, a brain injury for traumatic brain injury can cause a quick impairment of glucose utilization of the brain. By internalization of the GLUT3 transporter and also inactivation or reduced activity of Pyruvate dehydrogenase complex, the PDH complex, can be impaired under certain conditions of brain injury. Even certain viruses that cause neuroinflammation can impair this rate-limiting step for glucose metabolism.
So, alternative energy substrates are a way to bypass that glucose block.
(26:37)[Damien Blenkinsopp]: It’s like a diversification strategy?
[Dominic D’Agostino]: It is, in diving we always talk about being redundance. You need a level of redundancy to ensure safety. I think the brain does that pretty nicely. So we achieve that with fasting.
We have an alternative energy substrates being utilized in the absence of glucose. It’s interesting to be able to delve into that and understand what happens during fasting in different states. From my perspective, it’s a fascinating field of research to develop naturally derived or synthetic agents that can mimic those processes.
(27:17)[Damien Blenkinsopp]: Right. Because we are on a ketogenic diet do we also use fatty acids directly for energy substrates or do they have to be turned into ketones first?
[Dominic D’Agostino]: Yeah. Hepatic gluconeogenesis will be in a state of fasting, completely dependent upon the liberation of fatty acids from adipose tissue. Fat mobilization is directly almost correlated to a ketone production in that fasted state.
Our heart can use fatty acids more efficiently than glucose – our heart is an awesome fat burner. The skeletal muscle is an awesome fat burner especially in the keto-fat adapted athlete, the liver, various organs can use fatty acids quite efficiently. The long-chain fatty acids do not readily cross the blood-brain barrier.
Short chain fatty acids do, and medium chain fatty acids can actually cross the blood-brain barrier. So, that was actually an interest of mine and we did some brain metabolomic studies where we took out the hippocampus of some rodent models that we looked at. We saw a high level of the C8 and the CA10 MCT that we administered to the animals.
I think if you look at the ratio between the blood levels and the brain levels. I think there was a kind of like a 1:5 ratio, so that wasn’t readily getting through but a lot of it was getting into the brain. Of course, the brain was metabolizing it.
Our numbers might have not correlated precisely in a 1:1 ratio in that way. But it’s clear that our body can use fatty acids as fuels, and it’s an incredible fuel for our mitochondria. Because it metabolized exclusively in the mitochondria through oxidative phosphorylation.
(29:03) I would say ketone molecules are I’d like to call water soluble fat molecules, sort of an excessive beta-oxidation or accelerated beta-oxidation in the liver, contributes to the accumulation of acetyl-CoA which drives ketone production, and hepatic ketogenesis. So the acetyl-CoA essentially condenses to form acetoacetate. Then beta-hydroxybutyrate and these spill into the bloodstream.
So it’s interesting that the liver is a massive ketone producer but it lacks certain enzymes that prevent the liver from using the ketones as an energy source so it lacks succinyl-CoA transferase for example.
So, the liver will produce massive amounts of ketones. Then dump it into the bloodstream primarily for our central nervous system to maintain energy flow to the brain, then the central nervous system, and probably the heart too. The liver is a greedy organ, if you fast and you eat, the amino acids and glucose will basically stay in the liver and the liver will take what it needs and put whatever is left into the bloodstream.
But with ketones since the liver does not metabolize ketones it puts them immediately in the bloodstream when it’s burning fat for energy. Looking at it through an evolutionary lens, that function is to ensure that our brain gets adequate fuel flow. In the absence of food, if our brain tanked because we’re hypoglycemic, we wouldn’t be able to hunt.
So, being very lucid and having our brains energized during a period of food deprivation ensure that our species survived. The humans that weren’t able to do that did not get on and live. I think we’re sort of hardwired in a way to function optimally when we’re in a fasted state and that’s important to recognize.
Also, in the context of a society that’s programmed to give three high carbohydrate feedings per day. The metabolic program that is activated during fasting is largely silenced because of the societal norms, associated with our macronutrient profile, but also our eating pattern which is frequent feedings throughout the day.
(31:22)[Damien Blenkinsopp]: Yeah. One of the reasons I ask this is because I’ve had some fear and scared feedback about fasting for instance, which is a bit more of an extreme situation like ketogenic diet normally. One of the things I did was publish some of my own information on YouTube and I got some crazy comments from people saying I was going to die because my glucose was low.
I think it was 3.3 millimolar or something about 54-55 mg/dL. My mother’s a nurse and she saw the numbers and she was quite shocked at the time as well. Everyone thinks that we’re driven solely by glucose metabolism that’s the only thing they look at. So I think it’s really interesting that we have several various fuels that we can be going on, turns out that the glucose isn’t that important.
Someone else just sent me the numbers recently and they were the lowest I’d ever seen, like I was doing a fast and she got 1.8 millimolar with her glucose. I don’t know if you’ve seen anything that low.
[Dominic D’Agostino]: I did. Well, when I fasted for a week I tried some strategies, I probably shouldn’t talk about it here.
[Damien Blenkinsopp]: Okay. In case someone else does it.
[Dominic D’Agostino]: Yeah. After fasting a week, I was staying around the mid-fifties to low fifty’s and occasionally I would dip into the high forty’s depending on my activity and things like that. I did some strategies — I’ll label it as “strategies” — to lower it down to a level that the meter didn’t read, so it just actually was flashing low.
The lowest my meter was able to read was 25 or 26 mg/dL. I assume 25 that’s the limit. I spent a good part of the day with it flashing low and unable to read. I was using the Nova Max meter, and I was using the Precision Xtra Meter and also using the Neo Meter, so I had three different meters and I was scrambling.
[Damien Blenkinsopp]: Is that the Freestyle Optium Neo?
[Dominic D’Agostino]: Yeah. The freestyle like a lower profile sort of meter than the Precision Xtra. So I had three different meters, and I was measuring and I was like, “Oh no I don’t even know what my glucose is. All I know it’s probably under 1 millimolar range.”
I was starting to feel a little bit — using different pharmacological strategies to lower it — but I realized that I was at a level that was universally fatal for everyone if I didn’t have my ketones elevated.
[Damien Blenkinsopp]: Right. But if you had been admitted to the hospital, they’ll put you on the emergency ward most probably if you walked in like that.
[Dominic D’Agostino]: Yeah. During this particular day, I was preparing for a lecture, I was writing a grant it was really a productive day. As I was working I was doing these things and I would do measurements and work for a little bit more and it just goes to show it was a very dramatic demonstration an alternative energy source.
For me, that has tremendous implications therapeutically for someone that’s experiencing insulin shock or a neurological disease with impaired glucose metabolism. So we worked very closely with the glucose transporter type 1 deficiency association. It’s a rare disease where the brain does not have glucose available due to deficiency of the GLUT1 transporter.
There are many different diseases like that. I was also inspired by the work of George Cahill, there was a study that was published in 1967. The first author was Oliver Owen and they fasted subjects for 40 days.
In another report that wasn’t originally published with the original report. I found it in another book they administered insulin, 29 IU of insulin they gave IV. In these fasted subject they lowered the glucose down to 1-2 millimolar and kept it down there.
[Damien Blenkinsopp]: So it’s like 35 mg/dL somewhere around there?
[Dominic D’Agostino]: It’s not even that it was about that 25 range that my meter couldn’t read. So one millimolar would be 18 mg/dL. That inspired me, I was thinking if these subjects can fast for 40 days I could do a week.
It’s about five years ago or so that’s when I did the week long fast and did some experiments on myself. One of the most interesting things that happened to me was my breath hold time. So at the time I was outside a lot.
I was in and out of the pool, taking short walks and trying to stay active, keep my mind off of food. Because the main challenge was just the pleasure of eating was not there. I was swimming I was under the pool and I realized, “Wow,I had been down for quite a while”, and I wasn’t gasping for air.
I got back up to the surface and my girlfriend was there at the time, now my wife, and I started testing my breath hold time. I was like, “Keep an eye on me.” Normally I could do over a minute about 90 seconds, but I was able to stay down for three to four minutes which is remarkable.
I don’t have any kind of specialized training. I’ve been wanting to take a freediver course. I know Ben Greenfield did and we exchanged emails when he was going through that because he was trying exogenous ketones. But I found that after one week of fasting, I had a profound prolongation of my breath hold time. I think that’s fascinating to me.
Fasting does definitely start to shut down your metabolism. I think my body temperature probably went down a degree or two so the metabolic demands just weren’t there. But I think our drive to breath has a lot to do with our CO2 sensitivity.
So there’s receptors in the ventral respiratory group and the ventral surface of the medulla that sense CO2 levels and drive the urge to breathe. We also have the carotid bodies, at the bifurcation of the common carotid artery that sends oxygen and CO2 and they also mitigate or they also play a role in the drive to breath.
I think there’re interesting mechanisms going on there. A desensitization in some way or in combination to just altering our metabolic physiology. I think that has some practical benefits for different sports, maybe military operations.
I want to study that a little bit further with adaptations that happen during fasting.
[Damien Blenkinsopp]: Yes, very interesting. I’m wanting to go and test that out with freediving.
[Dominic D’Agostino]: A number of other people have, I think I might have mentioned it once or twice very briefly, not as descriptive in other podcasts but other people went out there and did it.
I think Tim Ferriss did it. I’m not sure if he’d blogged about it yet but he sent me quite a few texts and emails just saying that dramatically enhanced his breath hold time. So, I’m pretty sure it’s a real phenomenon.
(38:15) [Damien Blenkinsopp]: Very cool, to kind of round that conversation off. I get these emails, like I said, some people are scared because they get injured in fasting particularly a very low glucose levels of 30-35mg/dL.
Do you think that’s something to be concerned about or is it absolutely no problem? Typically, they have ketones like six millimolar, somewhere around there at that stage?
[Dominic D’Agostino]: I wouldn’t recommend that for a long term sustainment of life. Because there are a lot of biological processes that require glucose: red blood cells, your kidney, certain immune cells, and even biosynthetic processes like the generation of certain neurotransmitters are in some part glucose dependent. I think it’s good to get into that level and I’m going out on a limb by saying this to be a mainstream sort of medical college.
I actually think it’s very good to be in a state of nutritional ketosis with sustained hypoglycemia for a period of time, and to do that at least once a year, preferably a couple of times a year. I think what really kicks on a genetic program that activates so many biological processes that I think could be protective from enhanced insulin sensitivity to autophagy, to activating a number of different genes. There’s certain ones obviously, ampakine is activated, mTOR is suppressed.
You put tremendous metabolic stress on glycolytic cancer cells or pre-cancer cells that we may have in our body, sort of an immune activation. I know Dr. Adrienne Scheck is doing some work with the ketogenic diet and she’s doing some elegant work on the immune activation, and from the gist of it and from other bodies of literature it supports the idea that the immune system becomes hyper-vigilant, to recognizing and attacking existing cancer cells when we put our bodies into the state of fasting.
Either prolong fasting or even the ketogenic diet. I think it’s good to do that sometimes. But say if you’re on the ketogenic diet all the time in the state of moderate ketosis and then you fast.
You probably won’t get the same benefits as a person who’s on a high carb diet and did a fast. It would be a lot harder for that person who is on a high carb diet to do a fast. It would be greater stress because it’s that relative change or that pulse.
Thomas Seyfried and I we’re going to work on, it was originally his idea. We talked a lot about this press pulse phenomenon for the metabolic management of cancer. The press would just be a mild state of nutritional ketosis and the pulse could be periodic fasting or some of the things that we’re interested in. Such as hyperbaric oxygen therapy that could be pulsed exogenous ketones to further allow for a greater hypoglycemic response.
Also, you could pulse various cancer-specific metabolic drugs like 2-deoxyglucose, or dichloroacetate, or 3- Bromo Pyruvate] could be used. The press would just be nutritional ketosis and that would metabolically compromise a lot of the highly glycolytic, which corresponds to highly aggressive cancer cells.
(41:41)[Damien Blenkinsopp]: When you say press that would be like something chronic that you’re doing?
[Dominic D’Agostino]: Yeah. We know that being in a state of nutritional ketosis causes suppression of the hormone insulin. The cancer cells that light up on a fluorodeoxyglucose PET scan, a FDG-PET scan. The PET [or PET-CT] scan is really the gold standard technique.
I would say when it’s coupled with the CT scan allows you to precisely locate where that hypermetabolic activity is. So the PET-CT is an incredible, gold standard tool to assess the location and aggressiveness of existing cancer cells. The greater the standardized values that are coming out, like 2.5 would be sort of the normalized value.
If you have a PET scan showing SUVs of a 100 or 250, those cancer cells are very aggressive.
[Damien Blenkinsopp]: So they show up as the big red and yellow blotches?
[Dominic D’Agostino]: Yes.
(42:47)[Damien Blenkinsopp]: Yeah, we spoke to Gene Fine on a previous episode he was talking about the PET scan.
[Dominic D’Agostino]: Oh yeah. Actually Dr. Fine, you probably know he did a study for 28 days. He did a study with a ketogenic diet and he selected patients based on their PET scans. The topic that I was going to touch on is that insulin suppression correlates with ketosis.
I think even the title of his paper didn’t even mention the ketogenic diet, it was something like insulin inhibition therapy can be used to target cancer. It didn’t even talk about the ketogenic diet. But if you read the paper, he basically used the ketogenic diet to suppress the hormone insulin as a therapy for managing these hard to treat cancers or people who have failed the standard of care.
So, that would be the press that I’m talking about. The ketogenic diet limits glucose availability to the cancer cells. It suppresses the hormone insulin which drives IGF-1, mTOR and other factors that cause cancer cell growth and proliferation. I don’t know if Dr. Fine talked about it, but he has a number of publications.
I was inspired by his work and I actually got us to look at exogenous ketones and the effect on cancer cells. We find that if you limit glucose, suppress the hormone insulin and elevate ketones, the ketones themselves have anti-cancer effects. So, we did a study, we published in the International Journal of Cancer.
The first author was my graduate student at the time, Dr. Angela Poff, she’s now a research associate following up on this work. We gave ketones to highly aggressive cancer cells that have a glioblastoma-like origin. When we grew the cancer cells in the presence of ketones, even in the presence of 25 millimolar glucose, it inhibited, it dramatically slowed down cancer growth and proliferation.
(44:47) We did a viability testing where we looked at live cells and dead cells and the ratios of that. We found significantly more dead cells when we grew the cancer cells with ketones even in the presence of glucose. The take home was that ketones were probably turning down or shutting off a lot of some of the glycolytic mechanisms and there’s previous reports suggesting that ketone metabolism can turn down glycolytic metabolism.
So, that would be the press.
[Damien Blenkinsopp]: It sounds like a signal even for the cancer cells?
[Dominic D’Agostino]: Yes.
[Damien Blenkinsopp]: For them to switch them off even if they can’t use the ketones?
[Dominic D’Agostino]: Yeah, we think so. Now, we need to mechanistically dissect those kind of signals that are happening with the ketones because they do high-level sciences. Our lab approaches things a little different. We don’t sort of identify a target and then work up from that.
We screen a lot of things at the top and find out what works. Then, once we found out what actually causes animals to live longer or produce a neuroprotective effect then we go and try to find the mechanism.
(46:00) [Damien Blenkinsopp]: That sounds like a little bit like the pharmaceutical drug research process where they screen many many molecules for doing something. Correct me if I’m wrong. It seems like maybe it’s an efficient process to find things that work by just screening a lot of things and then focusing on the things that are working.
[Dominic D’Agostino]: Okay. So, it’s a little different, with pharmaceutical companies they actually target a mechanism or a biological kind of process and enzyme.
[Damien Blenkinsopp]: So they’re all looking for an end result right?
[Dominic D’Agostino]: Yeah. We’re testing a bunch of things, we don’t even know how they work. We’re testing various ketogenic exogenous ketone formulas and we don’t even have the pharmacokinetic nailed down yet. We don’t even know specifically how they’re metabolized.
We feel that it’s really important to get this research done so we can get these therapeutic agents out there as fast as possible. We screen a lot in various agents, first in human or first in animal, and then we identify what works. But the mechanisms, the metabolism is incredibly complex.
What we find is that it’s not working through one particular mechanism, it’s many different mechanisms working in synergy. The ketogenic diet, you have an increase in the GABA to glutamate ratio or ATP production you have a greater bioenergetic potential of the mitochondria. You have more TCA cycle intermediates.
The list goes on and on. There’s a science paper showing that ketones beta-hydroxybutyrate is a HDAC inhibitor. We published a nature medicine paper showing that inhibits the NLRP3 inflammasome and that’s independent of metabolism.
(47:41)[Damien Blenkinsopp]: So it’s like a huge dynamic system? There’s no way you can see all of the mechanisms going on there? As you’re saying you looked for the end effects and then you started looking for the mechanisms.
All of these mechanisms that you just brought up and started piecing them together to see how it worked after you’ve got the end result that you wanted.
[Dominic D’Agostino]: Yeah. The important thing is that it works and then the secondary important thing is to find out the mechanism. Because once you do know the mechanism, if the majority of the therapeutic effects or performance enhancing effects are due to a particular mechanism, out of many mechanisms. Then we can tweak the molecule of the formula, the pharmacokinetics, to further enhance that particular mechanism.
Then we can go back and tweak the formula, or the molecule to make it hydrolyze faster or to increase the sustainment of it, or deliver it in a certain nanoparticle formula to a particular tissue or something like that.
(48:37)[Damien Blenkinsopp]: So we’ve already spoken about quite a variety of basic applications, benefits of ketone based metabolism, and ketones. Could you just go through the top ones in your mind, maybe the ones that we haven’t already covered? So I know a lot of people are focused on weight loss for instance.
[Dominic D’Agostino]: That probably goes back to what they call the ‘Banting diet’. That even predates some of the work that I first got attracted to in epilepsy. So, epilepsy that would be the big thing.
The ketogenic diet, the only thing that is used for standard of care in mainstream medicine is the management of epilepsy. I always harp on this too, the ketogenic diet is grossly underutilized as a tool for managing epilepsy because it works when drugs fail.
It works in about two-thirds of the population. Imagine the efficacy of it if it was the first line of therapy. If you have a child that’s two or three years old and you load them up with anti-convulsant drugs, we know that these anticonvulsant drugs cause developmental delays. It’s even more important in pediatric epilepsy, I think to start with the ketogenic diet.
I just like to throw that out there. We’ve already talked about epilepsy. So, epilepsy would be the big one and obviously weight loss. You have the original Banting diet. Then Atkins came out with what he said was his famous diet but it was really a playoff with the Banting diet. It allows for effortless weight loss because when you’re in a state of nutritional ketosis the ketones function to control appetite.
It prevents your appetite from controlling you. We don’t really know the mechanisms that regulate appetite control, are incredibly complex. But we think that the ketones are essentially telling the brain it’s in a fed state, that’s the simplistic way to put it.
(50:32)[Damien Blenkinsopp]: Okay. Ketones get converted back into fat? Because people know that you basically pee ketones out when you first get onto a keto diet. Is that one of the mechanisms also?
[Dominic D’Agostino]: Well, yeah. If you collect all the urine of someone that’s on a ketogenic diet and then you look at how many calories are there, it’s pretty marginal. I think Atkins even advertised, “Look you’re peeing out fat, you’re peeing out calories.”
But it only came down to like 50 to a 100 calories or something like that. I think the big effect, the metabolic advantage really, is not that you’re burning more calories. I think there’re different organizations out there that we’re trying to prove if there’s a metabolic advantage to being in ketosis.
I think the big advantage that we need to focus on is appetite regulation. Our current diet of processed carbohydrates contributes to appetite dysregulation. The ketogenic diet is very effective at restoring sort of normal appetite behavior because there’s no fluctuations in blood glucose.
If we’re on a carbohydrate based diet and we go hypoglycemic that’s going to trigger an intense craving for carbohydrate re-feed to re-establish that glycemia. That’s completely abolished on the ketogenic diet.
So when you’re on a well formulated ketogenic diet, the craving that you’d have with hypoglycemia is going to be significantly attenuated if not abolished. We talked about weight loss and type 2 diabetes pretty much every disorder out there. Let’s think cancer, even kidney failure, neurological diseases like Alzheimer’s disease and many other pathologies are sort of linked pathophysiologically to the metabolic dysregulation and also obesity type 2 diabetes.
If a diet does promote a healthy weight loss and sustainment of that weight loss, it’s going to be therapeutic for many other disorders. Some of the things that we study include Alzheimer’s disease, ALS, we have a really active cancer research program in the lab. I have two Ph.D. students right now studying.
One is looking at Metformin and other cancer-specific metabolic drugs but combining it with a ketogenic diet. His main thing is to locate drugs. But we think some drugs will synergize with the ketogenic diet.
In another project is looking at the ketogenic diet or exogenous ketones and branch chain amino acids to mitigate cancer cachexia, which is muscle loss or wasting, so we’re looking at that. Exercise performance we’re looking at that. The most recent data that I’m really excited about because of the pretty robust effect as far as some of the behavioral models that we use.
One particular model is the elevated plus maze which looks at anxiety. We found that being in a state of nutritional ketosis that was induced completely with exogenous ketones stimulates in the elevated plus maze which is like a rodent going out on a catwalk. You can go into a cave or come out into an open area where you’re on a plank and you’re elevated in the air.
It’s a very anxiety producing situation. In our rodent models validate as a very useful model. We’ll spend much more time on the open arm and less more time hiding in the cave. We think that has significant implications for military personnel with PTSD and anxiety in general, and a lot of depression too is also sort of a comorbidity there with anxiety, a lot of depression, and anxiety fueled.
[Damien Blenkinsopp]: You’re saying that they’re willing to go out walk on the plank, take that risk and feel comfortable with it?
[Dominic D’Agostino]: Yeah.
(54:28)[Damien Blenkinsopp]: Do you measure it by time spent on the plank?
[Dominic D’Agostino]: Yeah. Less anti-social behavior I guess. We set up this elevated plus maze and then we have a whole video imaging system above it. We keep the animals as low stress as possible.
We have the same person working with the animals so they’re not experiencing different smells, and things like that. The room is very very quiet. We pay attention to circadian, light on light off things.
There’s a lot of variables that need to be controlled and then we image them in the absence of ketones. We see how much time they’re like in the middle, in the open arm, closed arm and our video camera system sort of can track all that. We have various programs and algorithms that do all the calculations for various things.
We do a bunch of animals just on a standard high carb diet. Then what we’ve been doing is testing various ketogenic agents, or various exogenous ketone and ketone formulas that would be administered 30 minutes prior to being put in this elevated plus maze, and being there for a couple of hours. Then we’ll track all that information, it’s all done blinded.
We have one person who’s, usually two people part of the project that’s administering the agent. The person that does the analysis does not know what the animal is receiving. We’ve got a pretty robust effect with a few of the ketogenic agents on reducing this anxiety behavior.
That’s some new data that we just presented literally less than a week ago in Budapest. That’s what I’m just returning back now. So we want to follow up on that. We used one dose, we need to determine what would be the optimal dose.
There’s a lot of work that we still need to do to optimize that and maybe think about putting together a formula that could be beneficial for people.
(56:30)[Damien Blenkinsopp]: Very cool. One of the ones you didn’t mentioned is Parkinson’s, is that something?
[Dominic D’Agostino]: Yeah. There’s an earlier study I think that was done by Dr. Theodore B. VanItallie. Dr. VanItallie is like 96 years old. We still communicate on the phone and through Email.
He was one of the original ketogenic diet researchers. He did a small sort of pilot study showing that people with Parkinson’s disease can follow a ketogenic diet and that being in a state of nutritional ketosis reduced the tremors associated with Parkinson’s disease and prevented some of the symptoms. Not a cure, but it could help manage some of the symptoms associated with Parkinson’s disease.
There really hasn’t been a good follow-up study to that. I know there was a ketone ester that was developed at NIH and a study at Oxford. There was that group that had a clinical trial open. But I think they might have had some problems recruiting people into that clinical trial, that opened a few years ago.
I know there was a clinical trial looking at the effects of exogenous ketones on Parkinson’s disease. And if we weren’t tied up with so many other projects I would be jumping on that. Because I was able to observe on Alzheimer’s patients when they took a medium chain triglyceride supplement, or even exogenous ketones. They would have pretty dramatic tremors.
And some Parkinson’s disease-like symptoms can be manifested in people with Alzheimer’s, especially advanced Alzheimer’s. I was able to observe and also got feedback from caretakers that when they induced a state of nutritional ketosis it really rapidly stops the tremors associated with that. So, that needs to be followed up on.
The pharmaceutical industry dictates a lot of what studies are done. Because you need a strong financial backing on top of a university, or chain of universities that supports this kind of research. On top of a review board, an IRB, that will prove this kind of research using these nutritional metabolic substances. There are many hurdles that need to happen.
Then you have to recruit patients on top of that and convince them that it’s not a drug but it’s a nasty tasting food that could potentially benefit you. They were like — well, it’s easier for a child, a son or a daughter [who] is bringing in their mom who is typically in a situation — 80 or 90 years old.
They’re not going to want to try to formulate some nasty tasting shake to do that. It’s much easier to just give them a pill. These are some of the things you see, the feedback that you get from people who are trying to implement these kinds of nutritional protocols in patients.
There’s a lot of hurdles. A lot of people ask me, “Well, if it’s so effective, how come science is not using the ketogenic diet or exogenous ketones to treat all these disorders?” I could write a book on the reasons why, but nutritional research is so hard to do.
Because nutrition is really tied into the lifestyle thing, and getting institutional support, getting the expertise needed, ensuring that patients are following through and complying with the protocol. All of these things are hard to do. A supplement, in theory, is a lot easier but we’re at the very initial stages. Because these are just new entities that just developed.
(1:00:16)[Damien Blenkinsopp]: Right, it’s only two and a half years you’ve had the ketone salts for instance, and the esters a bit longer?
[Dominic D’Agostino]: A little bit more than that. I would say the ketone ester was actually developed probably about 20 years ago, if you look into the animal literature. Then they were dropped because it was thought that they’re very expensive to produce and they taste like jet fuel.
Some of the people that originally developed these things, like Henri Brunengraber. He’s like a hardcore metabolic physiologist-scientist who develops a lot of remarkable things. But he kind of drops it and moves on to the next thing.
There’s also sharing the chair of his department and running a billion other things at the same time. So, I dug up some of this research and realized, “Wow, why didn’t anyone follow up on this?” Then I saw some of the work that was funded by DARPA, showing that they were the secret project.
They were using these ketone esters for warfighter performance enhancement. I found some patents and some files on that. I was like, “Well, this is what I need to explore, for use of CNS oxygen toxicity.”
Not only can the ketones potentially mitigate the oxygen seizures but the ketogenic diet was super effective. Even independent of the ideology of the seizures that it tends to work which is really remarkable. But instead of giving an anti-convulsant drug to a warfighter, which can dull your senses and impair your physical and cognitive performance.
You could be giving an anti-convulsant neuroprotective substance that enhances the physical and cognitive performance. It seemed like a win-win situation. I’d rapidly grasped this idea and just went into this manic state of writing grants and writing proposals, and digging up all the research.
Then, I was calling my program officer and I was like, “You need to hear this information and what I’m going to tell you.” We actually had a little meeting at our university and he was like, “We have to do this.” He was very generous to fund some of the initial basic science proof of concept research that demonstrated the efficacy of this ketone ester in mitigating oxygen toxicity.
It worked better than anything we had ever tested or anybody had ever tested, even drug wise. That’s going back in 2009 or 2010. From there, I’m really in safety because I’m really scared about bringing something to market that could potentially harm someone. I know there has been some discussion out there about the quote and quote dangers of a racemic beta-hydroxybutyrate salt.
People need to recognize the difference between someone’s opinion and scientific fact. The scientific fact is that racemic beta-hydroxybutyrate salts have been used for decades for treating a disorder called MAD, Multiple acyl-CoA dehydrogenase deficiency. I get Emails from the patients or from the parents that are treating their kids with this, and it’s like a miracle for them.
I also get Emails from parents that are treating their kids with glucose transporter type 1 deficiency syndrome with a racemic beta-hydroxybutyrate (sodium beta-hydroxybutyrate), which is actually a prescription you can get in Europe.
But they’re also using these commercially available ketone salt products which would be the ones that you might be familiar with. There’s KetoCana from KetoSports, Pruvit makes Keto OS, Forever Green makes Ketopia. The Kegenix product which is the one I’m testing now. It’s a really excellent exogenous ketone product.
This idea which was talked about in various podcasts, I think in Bulletproof podcasts and Ben Greenfield’s that racemic sodium beta-hydroxybutyrate was dangerous and ineffective. It is an opinion and there’s no science to back it up.
If you go back and listen to the podcast you’ll hear the speaker actually reference no actual studies. So, it has an intellectual property supporting the non-racemic, so that needs to be acknowledged and appreciated.
What is appreciated from my end, the science backing up the efficacy and the safety are really profound – like I’ve said on expert panels to approve some of these molecules. And no toxicologist or physiologist could find any evidence that racemic, which is the DL version of beta-hydroxybutyrate, was dangerous in any way.
For example, if you’re a medical doctor or a combat doctor on the field and you’re treating soldiers that have a loss of blood or you’re in the emergency room just talking to the ER doctors, use the Ringer’s Lactate and that’s Racemic lactate.
So, L-lactate would be the natural lactate that you would find in your body. The DL would be in an enantiomer or a mirror image of that lactate. Both of the lactate molecules get metabolized to energy. So, the same things happen with ketones. So the D and the L version get metabolized to ATP, to energy.
A lot of the metabolism has been worked out with very elegant tracer based fate association studies by Dr. Brunengraber at Case Western. Lactate Ringer’s has been used in millions of combat troops and emergency rooms. If there was a danger to using a racemic metabolate, there would be a lot of dead bodies around – and that has not been the case.
Actually, it’s FDA approved, it’s widely used and accepted, and it was even studied the difference between L-lactate and Racemic lactate before it became a standard of care. Actually, it was looked into, and it had exact same effect.
So, if you use the Racemic versus the L-lactate have the same effect at preserving the metabolic activity of the tissues and being protective in that way. So, that needs to be acknowledged that when statements are made, that they could be an opinion and not validated by scientific facts.
The ketone supplements that are on the market now that I’m aware of are very safe and from feedback, they’re very effective. I don’t support any particular ketone supplement that’s out there. I’ve tested all of them and they tend to elevate my beta-hydroxybutyrate and the .5 – 1 millimolar range for one dose.
So, for me to really boost my ketone levels up, I have to take a packet and a half, or a dose and a half, which I can tolerate pretty well. But I think there’s a lot of room for improvement and the products that are out there.
I hope to work with these companies, hoping that they will fund research to support the further development and evolution of these products for different applications.
(1:07:30)[Damien Blenkinsopp]: Excellent. Thanks for going through that because that’s something I have my eye on as well and wanting to get some more facts. Something else that was thrown out, a couple of things was that the racemics were less efficient or were ineffective?
We also have all of the MCTs which people are using to kick up their ketones as well. We have the C8 and C10 of the MCTs, there’re various products around. Another statement that was said they were undesirable and you should avoid those as well unless you really had to take them.
For instance, if you have Parkinson’s it was okay to take them but otherwise you shouldn’t be really taking them. But a lot of people are taking these. Right now, there’s a bulletproof brain octane. I’m sure a lot of people are taking that.
KetoSports has got their own product that I’ve been taking for a long time personally. I don’t know if you have got any comments on that?
[Dominic D’Agostino]: Yeah. I study a lot of very expensive exogenous ketone products. But the more I look into medium change triglycerides, especially the C8 oil which is digested and assimilated much differently than long-chain fatty acids. When you consume it, it basically perfuses the liver.
I mean it goes right to the liver via hepatic portal circulation. It goes right through to liver and is burned as energy. So, they’re poorly astrophied, which means they’re not re-astrophied back and packaged into chylomicrons, like long-chain fatty acids.
Once they reach the liver, it’s basically an obligate oxidation. The medium chains are almost completely oxidized to ketone bodies. Some of them will spill into the bloodstream because we find them in the brain tissue and other tissues.
But it’s independent of the various transporters too. For the medium chain triglycerides to get into the mitochondria there’s various CPT-1, for example, is not needed to get the MCT into the mitochondria. So, they bypass a lot of these rate limiting steps.
And you consume them, it goes right to the liver, you generate a lot of beta-hydroxybutyrate and some of that gets into the bloodstream. So you have the combination of ketones and the medium chain triglycerides going right to the mitochondria. And that can be very therapeutic and beneficial for many different disorders.
You have to realize that the person making that statement that MCTs are dangerous or ineffective, has some underlying personal interests in advancing the commercialization of his particular exogenous ketone, and that needs to be appreciated and understood.
From our perspective, we’re interested in testing that particular ketone formulation and 20 other, and finding out the truth, finding out which is most effective, which is safe. When it comes to the racemic, and the statement that racemic beta-hydroxybutyrate is not as effective. We have not found that out to be the case.
Actually, the first ketone ester that we studied for oxygen toxicity was a monoester of the R-beta-hydroxybutyrate we have formulated. And that did not prevent CNS oxygen toxicity, which actually was very strange to me. But the more research I did I found out that you needed to elevate both the acetoacetate and beta-hydroxybutyrate in the blood to mimic some of what happens naturally, physiologically.
The acetoacetate through spontaneous decarboxylation to acetone, or maybe it has it’s own metabolic effect independently. The elevation of acetoacetate was absolutely critical. It also in the presence of beta-hydroxybutyrate but it was absolutely critical to elevating both ketone bodies to get the anti-convulsing effect.
We published that in the American Journal of Physiology and showed the pharmacokinetics and seizure work with that. So, we screened a lot of agents and found out the particular ketone ester that we found to be most effective was 1,3-Buntanediol acetoacetate diester]. So it was 1,3-Buntanediol that was racemic, so it would make racemic beta-hydroxybutyrate.
But even the non-physiological enantiomer gets broken down and converted to Acetyl-CoA and some of that goes back to the physiological enantiomer so it all gets broken down and metabolized similarly to Ringer’s Lactate which is used in millions of patients.
But the important thing about that particular molecule is that when it’s consumed orally it gets hydrolyzed and it rapidly liberates the acetoacetate. Then the 1,3-Buntanediol gets metabolized in the liver and elevates beta-hydroxybutyrate. So you have both ketone bodies elevated in the blood. We find that it’s absolutely critical to get a certain level of acetoacetate to get the anticonvulsant effect.
(1:12:30) One thing I didn’t talk about was Angelman Syndrome, which is characterized by impairment of motor function and also drug resistant seizures. It’s extremely effective in an animal model of Angelman Syndrome.
If you look at Angelman Syndrome and the ketogenic diet, you come across case reports showing that it basically puts Angelman syndrome patients into remission, at least for seizures. So, it’s highly efficient for that.
So, the first ketone ester we studied was this R in the enantiomer, the hydroxybutyrate, and it was not effective. So it was actually the racemic version of a ketone ester that was most efficacious.
But we’re interested in exploring all different pathologies and finding out which one. So, we have not found out that the R and enantiomer is any more efficacious for any other disorder than the racemic. I think that’s important to acknowledge.
We also found that medium chain triglycerides tend to formulate really well with this exogenous ketones. Not only are they carriers but we think they enhance the transport across membranes and they improve the pharmacokinetic profile, two of many of the ketones salts. So when it’s formulated with MCTs which have the nice advantage of also being ketogenic.
One of the benefits of racemic, the other enantiomer, so there’s D and L. The L-enantiomer tends to impact the liver in a way that reduces hepatic gluconeogenesis. So, you have this hypoglycemic effect that is very well characterized by our laboratory and other peoples laboratory.
[Damien Blenkinsopp]: So you’re saying that ketones go up and the glucose goes down?
[Dominic D’Agostino]: Yeah. It’s more pronounced with the racemic and we don’t know why that is.
(1:14:22)[Damien Blenkinsopp]: Is that beneficial to some of the applications more than others? Weight loss for example?
[Dominic D’Agostino]: Yeah for weight loss, maybe for seizures too. We know that reducing glycolytic metabolism can be beneficial for seizures but also for cancer. As I mentioned, we have pre-active cancer research program.
The lower we can get glucose or glucose response to a meal, the lower we can reduce that, the better therapeutic efficacy we think the agent will have. If we formulate the agent with food, so every time our animal models will eat the food they’re getting a dose of it.
Instead of injecting into the animal or ‘gavaging’ it in the mouth for our cancer studies, we actually take these ketogenic agents and formulate it to about 10 to 20 percent of the weight of the food. Then we count the macronutrient ratio, and then they eat it.
Every time they’re eating the food they’re getting a dose of ketones with the glucose. Because we do a lot of our studies formulating with a high carb diet. Because we want to find out the therapeutic effects of the particular agent and distinguish that between the ketogenic diet.
But we also published a study, about a year ago, where we formulated the ketogenic diet with the ketogenic agent. We did this with a ketone ester and found that it further enhanced the anti-cancer effect of ketogenic diet.
(1:15:48)[Damien Blenkinsopp]: Okay. I’ve got a few questions about this. There’s some MCT powders on the market which combine glucose. Me coming from a ketogenic perspective, that’s not something I want to take with the MCT powder. There’re other powders which don’t have the glucose.
Is there anything to think about or is it not really an issue? Because there’s this effect of the ketones pushing down the glucose anyway? Would it have zero effect? I haven’t tested it myself yet.
[Dominic D’Agostino]: Yeah, the MCT powders on the market like Quest Nutrition?
[Damien Blenkinsopp]: Not Quest, they don’t. It’s basically the generic ones. There’s this cheaper one, generic one, where they’ll put glucose syrup in it and some other glycemic ingredients.
[Dominic D’Agostino]: Yeah, with my interest in the ketogenic diet and staying in ketosis, I would rather get my carbohydrates from things like vegetables, salads, blueberries and dark chocolate. Basically encompasses my carb intake there. So I would avoid that.
A staple product that I use, I have it right by me right now is the Quest MCT oil powder. I did a little bit of beta testing for them as they brought that to market. We went back and forth, and I tested that a lot.
I consumed a lot of that and I did tons of the blood work and got to the point where I was really impressed with the product. There’s not too many products that I consider staple products, maybe about a half a dozen in total that I keep with me all the time.
That MCT oil powder is great, it’s very versatile. You could use it in baking, you could put in my coffee, you can add it to protein shakes to further boost the ketogenic profile of your shakes.
[Damien Blenkinsopp]: Do you take that with you? I take this stuff as well, I’ve got it right next to me as well in my coffee [unclear (1:17:32)]. What I was going to say is that you take that on top of your ketogenic diet?
But I think an interesting thing, I talk to people and they’re taking the exogenous ketones or the MCT powder as a normal diet, or the body builder’s diet where it’s high protein, and they’re not doing a keto diet.
Then there are other people who are interested in getting keto but finding it difficult. They’re using it to ease into the keto diet. So there’re a couple of different applications people use them for different things. I’m just wondering what you’re ideas are in those scenarios.
Dominic D’Agostino]: Yeah. If I put the Quest MCT oil into my coffee or shakes or things like that. I generally try to avoid liquid meals, because liquid meals digest totally different. The only liquid meal that I have would be my coffee, and I would put in some coconut oil and MCT on top of that.
Occasionally, I put in butter or coconut cream. I’ve been using coconut cream instead of full cream. The benefit is that I can elevate my protein a little bit more. I generally eat two meals a day now that I’m home and not traveling.
My meal in the evening is about twice the calorie count. So, I get about a third of my food calories in the morning and about two-thirds in the evening, but I get a lot of fat calories during the day I guess. Because I’ll make my coffee and whip it up and then bring it in a thermos, and drink that mostly in the morning. Then I’ll have a little kicker in the afternoon maybe.
That fat balm, I guess if you want to call it that and occasionally take some exogenous ketones too during the day, if I’m testing different products. It just adds to my total fat macronutrient ratio.
I probably get — with the coconut cream, the butter, and the MCT oil powder — probably get about an extra 100 grams of fat from that. So that allows me to eat a little less fat with my meal in the evening, and that makes it maybe a little bit more palatable because I could add some more protein.
On a typical schedule, I will do my physical activity in the evening. Then I’d like to couple that with a little bit higher protein intake.
(1:19:51)[Damien Blenkinsopp]: Right. So using the exogenous ketones or the MCTs to offset gluconeogenesis? Is that the idea?
[Dominic D’Agostino]: Yeah. This morning I had three or four eggs cooked in coconut oil. I usually have sardines, oysters, chicken, or steak from the night before. Then I’ll have a little bit of green vegetables cooked in fat, and that will be my breakfast.
It will be roughly under a thousand calories, somewhere around 800 – 1000. Then, I’ll get 1,500 – 2000 calories in the evening. During the day, I might even get an extra 500 – 1,000 just of fat or ketones.
I stay semi- fasted, so if I eat 6am or 7am I feel the best when my ketones get highest between like 3pm and 6 or 7pm.
(1:20:53)[Damien Blenkinsopp]: Okay what levels of ketones would you have then?
[Dominic D’Agostino]: I say high but it’s not really that high. In the morning when I wake up it’s maybe 1.0, sometimes .5 if I ate more blueberries or chocolate the night before. Right now, approaching noon, it would start to creep up about 1.5.
Then towards the end of my work day, I’m usually approaching about a 2.0 – 2.5 or somewhere around there. If I’m lucky I budget my time where I can go to the gym so I will be typically be working out. Then if I go home I’ll do some stuff, take my dog for a walk, do some sprints, and that’s when I feel most energetic – when I’m fasted, and in ketosis.
(1:21:40)[Damien Blenkinsopp]: Right, and you’re saying your blood ketones would be 2.5 or something like that and you’d feel that’s when you’re most energetic? Or you feel your best at that time?
[Dominic D’Agostino]: Yeah. I try to subjectively do this too. Basically, I would carry my meter, and I would be like, “When do I feel most energetic, and lucid?”. Then, I would measure my glucose and ketones at that point.
And I find that basically if my glucose is about 3.5 millimolar and my ketones are about 1.5 to 2.0 is when I personally feel the best, as far as energetic. So that would be a glucose-ketone index if we use the Thomas Seyfried’s calculation, of about 2.0. When you’re approaching 1.0, you’re starting to get into that therapeutic range.
But I think for all intensive purposes, for the normal person, if you keep between 2.0-4.0. It would be very abnormal for someone in a normal society to even approach that. If you’re hitting that then you’re doing really well.
You’re in an altered metabolic state. If you can sustain that, I think you’re going to get a lot of therapeutic and performance benefits from that.
[Damien Blenkinsopp]: So 2.0 – 4.0 in the GKI — glucose-ketone index — from Thomas Seyfried?
[Dominic D’Agostino]: Yeah.
(1:22:58)[Damien Blenkinsopp]: Which we covered in his episode in the past. Yeah, the only time I’ve got below 1.0 is when I’d be fasting. I’ve tracked full days as well, every half an hour I’ve tracked, it looks pretty similar to yours.
I’ve heard you say before that over 5.0 millimolar, in terms of ketones has some metabolic downsides. So, I was wondering about the ranges. Are there ranges that people shoot for between this 2.0 – 4.0 basically? You don’t really want to be lower?
Right? Say on the GKI, you don’t want to be going down to 1.0 unless you’re fasting or doing some pulse?
[Dominic D’Agostino]: Yeah, unless you’re really in a total fasted calorie restricted, deprived state, I think between 5.0 and 6.0. I think there was a report in a 60 day fast up to 8.0 millimolar. So that it may be beneficial there for just maintaining that energetic flow to the brain.
But if you’re on an isocaloric diet not calorie restricted. I think staying between 1.0 – 2.0 is probably good. If you’re mildly calorie restricted or maybe towards the end of an intermittent fasting, the fasting portion of an intermittent fasting day, approaching 3.0 may be optimal.
I based this upon thousands of blood measurements that I’ve taken and literally hundreds of blood measurements from other people. Between 1.0 – 3.0 millimolar I think is good. We’ve even seen it in animals, once you dose them up to about over 5.0 they start hyperventilating.
You create a mild metabolic acidosis that needs to be compensated for, so that you get the hyperventilation, they start getting even drunk and sedated, when you really start getting up there and has signs of ketoacidosis. In cases where they’re sedentary, that could be the reason. If you’re approaching 5.0 or 6.0 millimolar and you’re in an all-out sprint, you’re using that.
So maybe in the case of an athlete approaching the higher numbers could be beneficial if you train for that. But say you’re not trained for that and you dose up really high. Your body perceives it as a foreign acidic-metabolic substrate that has to neutralize, your bicarbonate compensates, and you have respiratory-renal compensation that needs to compensate for that.
I just had this discussion in metabolism and physiology with some people that I really respect. They were making the argument that anything above 4.0 or 5.0 is really going to be toxic to the body. I didn’t argue against that but we agreed upon — and there’s some pretty sharp minds in the room — anywhere between 1.0 – 3.0 was probably optimal.
As you know staying in 2.0 – 3.0 range is really hard to do with diet. But staying in a 1.0 range is pretty easy to do with a diet. I do a modified Atkins or modified ketogenic diet, and that’s pretty easy.
Then if I add a little bit of exogenous ketones or some C8 on top of that. I can easily boost that up to 2.0 – 2.5. I think that would give me a metabolic, performance, and cognitive advantage. I’m pretty sure about that.
So, that’s what’s exciting to me. So, not using exogenous ketones in the place of a low carb diet — but you might be able to do that too — I’m actually thinking about doing some experiment of getting off of my ketogenic diet for a period of time.
Not going super high carb but just being out of a state of nutritional ketosis and then adding supplements back in and then doing some blood work and see what happens there. I just haven’t got around to doing it because I enjoy eating ketogenic so much.
[Damien Blenkinsopp]: Right. Once you get into it for a while it’s like you don’t have to eat very often.
[Dominic D’Agostino]: It’s almost like I dread doing it.
(1:26:51)[Damien Blenkinsopp]: I was testing some of the supplements, the different supplements. I don’t think I didn’t do it very well. But what I was doing I was eating in the evening basically a high-carb meal lots of rice to put myself out of ketosis.
I did this for about a week and then tested different supplements in the morning. For the first reason, I don’t think it was a great control because I am basically keto-adapted now. I tend to pop straight back into ketosis relatively quickly.
I’d like your feedback on that whether it’s a decent control. Maybe I’m no good as a control because I’ve been just keto-adapted for a while and also may be I’d have to go for a few days ‘carbing’ it to make it a bit more realistic. What are your thoughts on that?
If you’re trying to do some normal, the first thing is, going back to your point about exogenous ketones. You’re saying like if someone just takes it straight off as some people are doing right now. They’ve been on a carb diet the whole time.
Then they can’t necessarily utilize those because they’re not keto or fat adapted. How long does that take? Should we be taking a lot of these when they haven’t really had that much exposure?
Do they have to take them over a period of a week or longer in order to start getting more benefits from taking them?
[Dominic D’Agostino]: Yeah, that’s a good question. Interestingly, we can use exogenous ketones even if we’re not keto-adapted at all, and that was our first study that we did for CNS oxygen toxicity. It was actually rats eating a standard rodent chow which is 60-70 percent carbohydrates.
We gave a single dose not even feeding it chronically, 30 minutes prior to doing a deep oxygen dive. It worked remarkably well and that really surprised me. So, taking a little bit of a step back, we use the R-enantiomer of the beta-hydroxybutyrate, and it didn’t work.
But then when we found out the ester that did work, that particular compound worked remarkably well. That kind of changed my thinking because I approached it with the understanding or the bias that you really need to be keto-adapted. But if you are adapted to burning fat and ketones for fuel, what has been shown is that you do up-regulate the transporters and the enzymes associated with ketone metabolism.
So, you will theoretically be deriving more benefit from exogenous ketones if you have been previously adapted to a ketogenic diet. I think from a practical standpoint, say you’re on a ketogenic diet and you choose to transition to eating carbs for some reason and then you throw ketones back in. Since you’re adapted to a ketogenic diet already, I think you’ll use those ketones more efficiently even by following a carbohydrate based diet.
We have some evidence to indicate that glucose disposal is enhanced in the presence of ketones. So, it may actually be enhancing insulin sensitivity. The glucose goes does, if you have animals eating a high carb diet and you bolus exogenous ketones, the glucose goes down remarkably low. Much more than you even get with something like Metformin.
What we don’t know why that’s happening, we want to look at the liver metabolimic profile. I think it could be influencing the liver in some way, and may be decreasing hepatic glucose output. Really it’s your liver that dictates your blood glucose, it’s all happening in the liver.
So, if you turn down gluconeogenesis in the liver, you would see a decrease in blood glucose. But also if you’re enhancing insulin sensitivity you would be facilitating glucose disposal and peripheral tissues with ketones. I know Dr. Richard Veech at the NIH has written about that and suggested that ketones actually do enhance glucose uptake and insulin sensitivity.
I get the question, what if you throw ketones on top of carbohydrates? What are the cells going to use? I think the cells will use what’s available to them and we know that the brain might not be able to use the certain types of fatty acids but they can use MCTs.
If you have glucose and ketones in the blood, your cells, your muscle cells, brain cells will be using both fuels. There’s some evidence that suggests that it will be using the glucose more efficiently in the presence of ketones. Because we know ketones can lower reactive oxygen species.
Excess ROS production can decrease insulin sensitivity and cause protein nucleic and lipid peroxidation that can inhibit glucose transporter processes. Even translocation of glucose transporters to the membrane or even PDH complex could be sensitive to the Redox state of the cell.
Ketones tend to normalize or prevent an oxidative environment that could potentially impair glucose transport and insulin sensitivity.
(1:31:56)[Damien Blenkinsopp]: There’s such a wealth of information in this area. It’s not like ketones are a panacea, but there’s just so many applications we’ve spoken about today, so I could go on talking to you for absolute forever. I’m conscious of your time also.
I wanted to round off of a bit of what you do more in terms of optimizing yourself and what you think is effective. For instance, in terms of blood ketones, you said you’re tracking your blood ketones. Have you used the other methods, the urine or the breath method?
The strips for the blood can be a little bit inaccessible in the UK, in the US sometimes, and also they are really expensive. The price varies. I’m sure you have your own ways of getting them but for everyone else it can be a little bit difficult, particularly in the UK I’ve found.
What do you think of the breath? There’s the Ketonix looking at the acetone instead. Do you think that correlates with the blood ketones, and it’s an okay way to try and optimize or not?
[Dominic D’Agostino]: Yeah, it’s a good question. I get this frequently. What I would say the breath, if you’re measuring moderate to high on a breath acetone meter you’re definitely in ketosis. I like it, and I wish it was more quantitative because I’m a numbers guy.
I think we’re all sort of what’s your number? There was like a ketone competition in the lab and my friends like, “You know what’s your ketones today?”. So we like numbers and I wish the unit could be designed.
I believe [unclear (1:33:20)] who’s working on a quantified meter. I like it, and I think it’s great for kids that are trying to manage their epilepsy because breath acetone has correlated with seizure control. So if you give this to a kid and he blows in it and he sees colors and he gets excited, I think that’s great.
It’s giving you a relative level but it’s not a precise level. But it’s also a snapshot of your level of ketosis over the last couple of hours. So your blood, beta-hydroxybutyrate can change.
I’m standing here in front of my desk and talking to you and relatively sedentary. But if I was to go and take a brisk walk on the other side of campus which I do occasionally to get things signed. I’ll come back and measure my ketones, and it’ll be cut in half.
It’ll go from two to one, or below one, just from brisk walk where it should be increased right? Because I should be mobilizing fat, I’m burning fat. But I’ve burnt those ketones for fuel during my movement.
(1:34:25)[Damien Blenkinsopp]: So then it goes into glycogen? I’ve seen this before and I didn’t understand it, that’s why I’m pretty curious.
[Dominic D’Agostino]: Well, it’s burned as fuel. Ketones are substrates, so they’re going to be burned up as fuel. And yes, you may mobilize glycogen from the liver so your glucose can actually go up. You might have some lactic acid from your muscles and through the Cori cycle goes back to the liver and you get some glucose in the blood.
The stress, the sympathetic nervous system from moving and running across traffic and navigating or whatever you do when you walk, that can contribute. What I really found that’s most important is you need to be completely calm and sedentary when you make these measurements to get accurate measurements to prevent the variability.
We have this issue with our rodent studies, we need to pull the food from them for about four to eight hours, to normalize the blood glucose. Because you have some that are nibbling on food, some that have gorged, others haven’t eaten. So the glucose is going to be all over.
To standardize and normalize glucose, you need to remove their food for a little bit and the numbers are tighter. The same thing applies for measuring ketones, especially blood ketones, you need to be fairly sedentary to do it. I really like the urine ketone strips, got a bad wrap, but I like the urine ketone strips.
They’re still used by John’s Hopkins. So, before you go spending a lot of money on getting ketone strips for the meter. You want to first confirm that you’re actually in ketosis on a urine strip.
If you’re registering 15 or 40 mg/dL on a ketone strip then it’s like, “Okay, at least if I take a blood measurement now. I’m going to register something on my blood meter and it’s going to be ‘I’m in ketosis’.” I remember the other meter, I think it’s the Novamax meter, would just give you this annoying, ‘low’, it won’t even read your number on it.
One person went out and bought a couple hundred hours worth of strips and have like 17 lows on there, and have come to find out you’re just eating too much protein or they think it’s okay to drink fruit juice. I forgot what the situation was.
Well first change your diet, then go out and get some urine ketone strips. Once you’re actually in ketosis on the urine strip then go back to the blood meter. And come to find that they tweaked their diet a little bit.
They did it until they were measuring ketones on the urine strip and they went to the blood meter, and bang they get 1.2 and they get all excited. So they could’ve saved a lot of money.
(1:37:04)[Damien Blenkinsopp]: Right. Because the urine gets a bad wrap, because it stops working once you get more keto-adapted. But when you’re first on a ketogenic diet and you’re trying to check that, that’s not going to happen. Right?
[Dominic D’Agostino]: Hydration state too, also plays a role, and less ketones will spill into the urine over time because you’ll conserve them as fuel. The transporters change a little bit. But if your hydration — if you’re drinking lots of water those people who carry water around with them and drinking.
Your urine ketones may register pretty low. Sometimes I wake up dehydrated and I would check my urine ketones will be quite high, whereas my blood ketones would be quite low. So, that’s just an indication of my hydration status.
It’s also a snapshot of what your ketones were over the last four, five, six hours because that urine is collecting in your bladder over time. So it’s sort of a snapshot of what’s happening through the course of the day, whereas your blood ketone is a snapshot of your ketone level at that point in time.
(1:38:04)[Damien Blenkinsopp]: Right, just a bit of information more about you and what you do these days? In terms of tracking things, it seems like you’ve tracked a lot yourself. Are there things that have stood out for you?
Overall, the time that you’ve tracked yourself and you found really useful insights from? Any quants or anything you’ve changed something you do in your life because of that?
[Dominic D’Agostino]: Yeah, I think initially when I started doing the ketogenic diet it was very dairy based. I was taking lots of creams, a stick or two. Two sticks of butter a day. So, I had a really high intake of dairy fat, probably about 200 plus grams of fat per day of dairy.
My LDL went up pretty high and my triglycerides went down a little bit but not really low. Then, I started replacing some of the dairy fat or the whole cream with coconut cream, and just using a little more coconut oil, getting more avocado in from my fats.
I still get dairy fat, by a sour cream that has live cultures in it. I’ll probably get about 50 to 70 grams of fat per day from dairy instead of like 250 grams of fat which I was getting initially. My lab test has improved. I guess you would say, I think my insulin sensitivity is better.
My glucose I can get lower glucose numbers now after eliminating some dairy. My triglycerides are really low now, they stay at 40s to 50s, I think it was 36 at one time. My HDL has improved and better and it’s really high, like 90 something.
My LDL went from really high to normal, but normal high. Now, which I think is completely normal and actually maybe even optimal. My IGF-1 levels are really low now compared to when I was on dairy.
I think dairy may have been contributing a little bit to some insulin resistance or maybe I was just getting a surplus amount of calories. My CRP levels also are the lowest now than they’ve ever been. I mean it’s like 0.1 or 0.2.
[Damien Blenkinsopp]: Right. Basically nothing, that’s the bottom of the range.
[Dominic D’Agostino]: Yeah, it’s like totally bombed out. I just feel better. If I eat a lot of dairy, I do wake up a little bit slightly congested, stuffy in my nose but it’s not bad.
I wouldn’t call it an allergies, and it could be due to allergies. But eliminating that has sort of helped, not eliminating, but reducing the amount of dairy. I don’t get in a whole lot of dairy protein. Maybe a slice of cheese here and there but I limit that. I limit casein. I don’t take away protein anymore.
The dairy that I get is primarily dairy fat. I was actually thinking about, I get very little butter, but I was going to switch to Ghee, and do some clarified butter. The triglycerides I would say for people to look at, for physiological biomarkers, your heart rate, blood pressure, sleep is an important one.
I wear the FitBit Charged. It’s really fun to look at my heart rate during the course of the day and in my sleep, and those sorts of things. I have a Dexcom that I’m going to put in. And I want to…
[Damien Blenkinsopp]: Is that the latest one? Is it the 4 or 5?
[Dominic D’Agostino]: Yeah.
[Damien Blenkinsopp]: I know Peter Attia is playing with that.
[Dominic D’Agostino]: Yeah, the 5 I think it is. So, I’ve just been traveling I just wanted to wait until I was put it in one spot and I can test it. I’m interested in trying that, and maybe working with some companies too, to do a glucose and ketone Dexcom.
I’m hoping to try that. That would definitely fit into your show. Yeah Quantified Self, and get some data for that, that would be good. As far as looking at physical biomarkers, you want to look at blood pressure, heart rates, sleep, and all these things improved when I got on a ketogenic diet.
I think there were various reasons for that. The lab test, the simple ones are probably the most beneficial ones. Triglycerides are the things that I look at the most. My HDL I think is important, and CRP, and of course your blood glucose. If you’re keeping glucose levels between 60 – 80, and doing that pretty much all the time.
Everything else is going to be good, that’s what I find.
(1:42:35)[Damien Blenkinsopp]: You said you did an insulin sensitivity, was that the homo or was it something else?
[Dominic D’Agostino]: No, I didn’t do that. I did the glucose tolerance.
[Damien Blenkinsopp]: Okay, the challenge.
[Dominic D’Agostino]: Yeah. I did like 50 grams, 75 and 100 grams I think. I think that was like over four hours, the 100-gram ones. Yeah, you drink the nasty Slurpee glucose and look at that. I’m extremely insulin sensitive. I dispose of glucose very fast.
I can also get a little bit of a hypoglycemic effect. If I’m on a ketogenic diet, and I go off of it. For example, I get some rice, sushi, or something like that, I will dip down into the low 50s and bounce back up again – very, very insulin sensitive.
(1:43:18)[Damien Blenkinsopp]: Thanks for that. If you were to recommend one experiment. I can guess what you’re going to say. So, we should try to improve the body whether it’s health performance longevity with the biggest payoff.
What would that be? How should they track it to make sure it’s getting that payoff?
[Dominic D’Agostino]: It depends on the person really. I don’t think low carb ketogenic diets are ideal for people in their teens or early 20s because they may be extremely insulin sensitive. I know I have tons of friends and I’ve even measured their glucose levels, and they’re great.
They stay pretty low, the glucose levels and they have adapted really well to a high carb diet. They wouldn’t want to do a ketogenic diet. So, maybe you’re expecting that kind of answer.
But, I think periodic fasting would be an important thing to do. I’ve been talking to some high-level CEO people and they tell me, “Well, I’ve been doing this anyway because I’m so busy. I wake up and I just work all day, and just go home and eat at night.”
But if your pattern of eating — like my patter of eating — I was obsessed with eating every two hours especially when I was really into lifting. I felt I had this preoccupation with food, preparing my meals, carrying it with me. I think it’s very liberating to not have to do that and to realize that your performance, energy levels, are not going to tank if you eat one meal a day.
If you were to do a short term fast, initially, and to do that every once in a while. I think, not only is very good for your metabolic health. I think it’s also good for your state of mind because it tells your body. It tells your mind that you don’t have to be sort of psychologically dependent upon food.
I would go five or six hours, and I’ll be like, “I’m starving I have to eat something.” I have been around people that are like that. My wife is kind of like that, she’s an incredible carb burner.
But if we’re traveling and she’s gone four to five hours without having a meal. I could see it in her mood and in everything. But that’s fine we’ll stop and get something to eat, and usually we’ll have coffee or something like that. But it’s interesting to see, and she sees it in me, “How could you go this long? Aren’t you hungry? What’s wrong with you?”.
She understands it now. She’s watched me do so many tricks and everything. If you’re not a big fan of being hungry. If you’re not a fan of having to eat every two or three hours because you’re hungry. I think doing some intermittent fasting would be a really good experiment for you to do.
I actually interviewed Mark Mattson at IHMC. So, I’m also a research scientist at Institute for Human and Machine Cognition. We interviewed Mattson, I think you did too for a podcast. He really went into the benefits of intermittent fasting and he’s at the National Institute of Health.
If you get a chance, he gave a brilliant lecture, presentation. If you go to IHMC lectures and look up Mark Mattson, he gave a great talk on this. He talks about all the health benefits.
If you do embark — if your listeners embark on [an] intermittent fasting experiment it would be interesting for them to track their blood glucose levels, their ketone levels, their triglycerides and their c-reactive protein. I think in each one of those biomarkers, if you want to call them that, will improve with intermittent fasting. I’ve seen it.
(1:46:51)[Damien Blenkinsopp]: You’re saying the 16-hour window or one day? Because you said short-fast, do you mean like a one day, 16, or 20 hours?
[Dominic D’Agostino]: Yeah. You could do every other day eating. But I think the easiest thing to do for most people would be, what I’d do if I do intermittent fasting maybe once or twice a week now. I eat two meals a day but like once or twice a week I’ll eat one meal a day, and it varies depending on what I’m doing and testing.
But it will be 18 hours of fasting and 6 hours of eating. Actually I get home late, so it ends being about 20 hours of fasting and four hours of eating. So, it will be 7pm – 11pm. I’ve done it [with] water and abstained from putting fat into my coffee.
I’ve also done what I would call ‘fat fast’, so I would put in some MCTs in my coffee and maybe get a ketone supplement during the day. I would still call that a fast because it’s basically non-glycemic.
[Damien Blenkinsopp]: Yeah, probably has very similar ketone and glucose effects.
[Dominic D’Agostino]: Yeah, I actually find that it’s optimal. So, I would call that a modified intermittent fasting protocol, where you would get in some fats and exogenous ketones during that fasting period. I’m a little less hungry once I go into that eating window.
I think that’s good too, so I tend to not over eat that much. My body is still strongly in a state of ketosis that has probably enhanced a bit with the supplementation. It tends to dampen my appetite a little bit so I’m not as ravenous.
But I don’t generally don’t get that ravenous anyway when I eat. But, I would experiment with that the intermittent fasting. I think it’s so easy to do. I mean intermittent fasting is easier to do than the ketogenic diet that’s what I find with people.
So, do some experiment, get some initial blood work, read up about it, listen to Mark Mattson’s talk on [the] IHMC website and you’ll find it there. I’m sure there’s a lot of blogs on the subject and do blood work before and three to four weeks after.
You’ll see pretty big effects, especially six and eight weeks after. You’ll see even bigger effects on your lipid profile and metabolic biomarkers.
(1:49:04)[Damien Blenkinsopp]: Excellent thank you so much for that, that’s a great one. Where would someone look to learn more about your topic? Are there any good books or presentations on the subject you’d recommend if they want to learn more about the whole subject of ketones and ketosis?
[Dominic D’Agostino]: One of the go to book that I would recommend is Jeff Volek’s ‘Art and Science of Low Carbohydrate Performance’. It’s a mandatory reading for students entering the lab just to get a hand on what the ketogenic diet is. The Ketogenic Diet Resource is a website maintained by a friend of mine, Ellen Davis, and I think has a lot of good information on it.
But I maintain a website to throw up links, compile links in there called ketonutrition.org. If you click on resources from the homepage, it will take you to dietary consultants, books, publications, list of podcasts, and lectures on there on a variety of subjects that hit on pretty much all the topics we’ve discussed. I probably need to get on there, but it’s relatively updated. I’ll probably update that in the next month or two.
Metabolic Optimization too, that’s a website that I started with Travis Christofferson who wrote the book ‘Tripping Over the Truth’ which is an excellent book that covers the metabolic theory of cancer. Travis and I maintain the website Metabolic Optimization, and we have Thomas Seyfried on.
We’ve had Adrienne Scheck, we’ve had Bruce Ames actually was our first guy. We’re going to line up a bunch of other speakers on metabolism so that’s another area where they can look up information on these topics.
[Damien Blenkinsopp]: Great, thanks for that. Are you active on Twitter? Where could people also connect with you and keep updated of what you’re at?
[Dominic D’Agostino]: I tried to post at Twitter maybe once or twice a week, not like super active. But on Facebook I post a little bit more. My page is maxed out, I got 500 or 5,000 people following me.
So I’ll probably create a more public page. But you could still follow me because I post things open to the public. I will post usually one or two studies per day, or podcasts or lectures per day on my Facebook page which should be very easy to find.
It’s always sort of topics relevant to the interests or the topics that we covered today. Sometimes I dual post on Twitter and Facebook, important things that pop up as far as studies and lectures and things like that.
(1:51:39)[Damien Blenkinsopp]: Excellent. Of course, we’ll put links to everything you’ve mentioned here in the short notes. Is there anyone besides yourself? You’ve already mentioned a few people, but was there any you would pull out and you would recommend if people wanted to learn more about the subject? Are there are some other people that you would recommend also?
[Dominic D’Agostino]: Yeah. My colleagues, there’s so many of them. I try to stay very active in collaboration. It’s really good for scientists to collaborate to help get their work out there. Also, to get other people to validate the findings that you did in the lab.
So, I know you’ve had Thomas Seyfried. He’s a great friend and colleague of mine. Adrienne Scheck is a fantastic scientist and a pioneer in ketogenic diets and moving the ketogenic diet into clinical trials at Barrow Neurological Institute.
There’s some of the mentors that even got me into this field — would be Dr. Eric Kossoff. He’s a neurologist at Johns Hopkins. He’s been a pioneer in using a ketogenic diet for kids with epilepsy, so look him up.
John Roe who’s a neuroscientist and pediatrician. He was originally at Barrow Neurological Institute and he was the first scientist I ever connected with to discuss this. The use of the ketogenic nutrition for oxygen toxicity.
Dr. Richard Veech he had a profound influence on me when I first got into this area of ketogenic diet and discovered exogenous ketones. It was his reviews on the subject. So if you look up on some of his reviews on ketones and the therapeutic effects of ketones, they’re really good.
Susan Masino has been really supportive of our work and she’s doing some really innovative work looking at the effects of the ketogenic diet on adenosine. Adenosine is a neuroprotective substance that’s elevated, has anti seizure, anti-convulsant, neuroprotective effects.
So, we actually have a lot of these speakers [who] will be coming to our Metabolic Therapeutics’s Conference which will be held either the last week in January or the first week in February. We had a number of speakers, we had Eugene Fine, Colin Champ, David Ludwig, David Diamond, he was a colleague of mine here at USF and [we] talked about cholesterol and statins.
We had Eric Kossoff, Adam Hartman, and a bunch of scientists. So, I would tell your listeners to go to the Metabolic Therapeutic’s website. We’re in the process now of sending out the invitation for speakers.
And pretty soon, I think we might have a preliminary site set up for that, but we’ll be updating that soon with all the different speakers and the topics that are going to be talked about. We really try to emphasize basic science, so you’re going to find lectures on neurophysiology, cancer biology, proteomics, tracer based metabolomics.
Performance — Jeff Volek will be there talking about performance. It will be a mix of things related to not just the ketogenic diet but metabolism in general.
[Damien Blenkinsopp]: Sounds fantastic so anyone can attend that?
[Dominic D’Agostino]: Anyone can attend that, yeah. We should have the registration going up soon. The problem that we had is that last year the venue was small. We wanted originally to keep it small, to cap it at about 250, but we had to turn so many people away.
So, this year we’re going to blow it up a little bit and probably have about maybe 600 – 700 people, hopefully in the same venue. But we’re going to get the whole hotel. You’re going to find a lot of great companies there that are producing these exogenous ketones.
So, Pruvit is going to be there, probably Forever Green, the company Kegenix – they make a great product that I’ve been testing recently during my travels. KetoSports hopefully will be there, and Quest Nutrition has a big footprint in our conference and they have been incredibly supportive of our work.
Scivation, who’s really the leader in branch chain amino acid supplements, will be there. Let me see, we have a lot of good sponsorship supporting this area of research. It’s really exciting to me that it’s becoming so popular it’s easy to find companies that are now emerging that are interested in developing products that can enhance nutritional ketosis.
So it’s fun to see a market for this evolving. They’re are creating products that I think will be very beneficial to patients even that are following nutritional ketosis for managing a disease process.
I do get Emails every single day from patients that are using these products that made a world of a difference. They couldn’t get into ketosis and once they did or their trial did, they started getting all these benefits from the ketones.
[Damien Blenkinsopp]: It’s a super exciting area, you’re very lucky to be right in the center of it.
[Dominic D’Agostino]: Yeah. I do feel lucky.
(1:56:48)[Damien Blenkinsopp]: Just as a quick anecdote, I gave some MCT powders and C8 to my mother because she has tremors. They have been getting worse over time, and they are so much better it seems. She was really surprised by that.
But it is an exciting area, they have so many crazy benefits, so broad compared to the other things we looked at. Which is one of the reasons I’ve covered it several times in different episodes, fasting, ketosis, all of these.
Whereas most topics I don’t cover in many episodes but this one has just so many applications, it’s just interesting. I think it’s worthwhile for people to learn more and more about it.
[Dominic D’Agostino]: Absolutely.
[Damien Blenkinsopp]: Dom, thank you so much for your time. I really appreciate it, we’ve covered such a wealth of topics. I know there’s so much more you could talk about. So, thanks very much for your time.
It’s been great talking to you.
[Dominic D’Agostino]: Thanks for having me Damien. I appreciate it.